Articles
Article Tools
Stats or Metrics
Article
Original Article
Exp Neurobiol 2020; 29(4): 314-322
Published online August 31, 2020
https://doi.org/10.5607/en20030
© The Korean Society for Brain and Neural Sciences
Higher Lactate Level and Lactate-to-Pyruvate Ratio in Autism Spectrum Disorder
Miae Oh1, Soon Ae Kim2 and Hee Jeong Yoo3,4*
1Department of Psychiatry, Kyung Hee University Hospital, Seoul 02447, 2Department of Pharmacology, School of Medicine, Eulji University, Daejon 34824, 3Department of Psychiatry, Seoul National University Bundang Hospital, Seongnam 13620, 4Seoul National University College of Medicine, Seoul 08826, Korea
Correspondence to: *To whom correspondence should be addressed.
TEL: 82-31-787-7436, FAX: 82-31-787-4058
e-mail: hjyoo@snu.ac.kr
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and
reproduction in any medium, provided the original work is properly cited.
Abstract
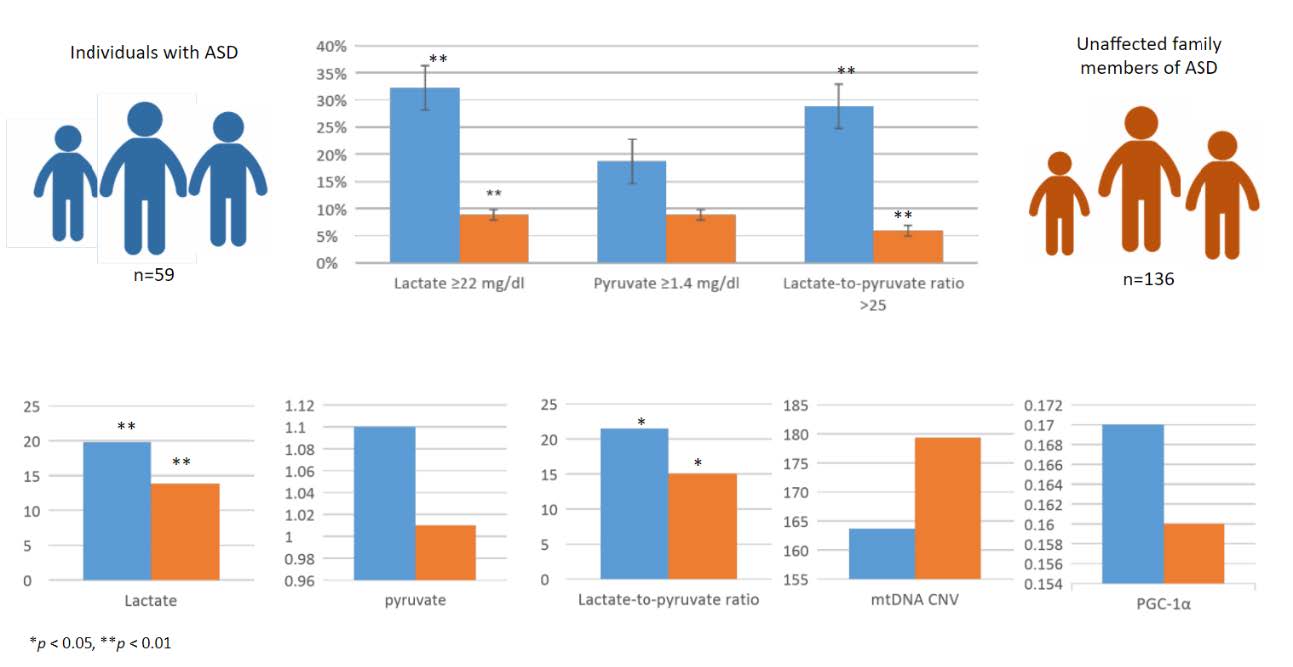
Mitochondrial dysfunction is considered one of the pathophysiological mechanisms of autism spectrum disorder (ASD). However, previous studies of biomarkers associated with mitochondrial dysfunction in ASD have revealed inconsistent results. The objective of this study was to evaluate biochemical markers associated with mitochondrial dysfunction in subjects with ASD and their unaffected family members. Lactate and pyruvate levels, as well as the lactate-to-pyruvate ratio, were examined in the peripheral blood of probands with ASD (Affected Group, AG) and their unaffected family members (biological parents and unaffected siblings, Unaffected Group, UG). Lactate ≥22 mg/dl, pyruvate ≥1.4 mg/dl, and lactate-topyruvate ratio >25 were defined as abnormal. The clinical variables were compared between subjects with higher (>25) and lower (≤25) lactate-topyruvate ratios within the AG. The AG (n=59) had a significantly higher lactate and lactate-to-pyruvate ratio than the UG (n=136). The frequency of subjects with abnormally high lactate levels and lactate-to-pyruvate ratio was significantly higher in the AG (lactate 31.0% vs. 9.5%, ratio 25.9% vs. 7.3%, p<0.01). The relationship between lactate level and the repetitive behavior domain of the Autism Diagnostic Interview-Revised was statistically significant. These results suggest that biochemical markers related to mitochondrial dysfunction, especially higher lactate levels and lactateto- pyruvate ratio, might be associated with the pathophysiology of ASD. Further larger studies using unrelated individuals are needed to control for the possible effects of age and sex on chemical biomarker levels.
Graphical Abstract
Keywords: Autism spectrum disorder, Lactate, Pyruvate, Lactate/pyruvate ratio
INTRODUCTION
Autism spectrum disorder (ASD) is a neuropsychiatric developmental disorder characterized by impaired social communication and a tendency for repetitive, solitary interests and behaviors [1]. The prevalence of autism has markedly increased over the past decades worldwide [2]. A recent study using data from the National Health Interview Survey reported that the prevalence of children with ASD aged from 3 to 17 years increased by 2.24% in 2014, 2.41% in 2015, and 2.76% in 2016 in the US [3]. However, because of the phenotypic and genotypic heterogeneity among affected individuals, the etiology of ASD is not yet known in most cases. For this reason, ASD is diagnosed clinically, and the absence of other diagnostic tools, such as biomarkers, can be a problem because the diagnosis may be delayed if symptoms are mild. Therefore, many researchers are searching for diagnostic biomarkers for ASD in order to aid diagnosis when the symptoms are not clear and during the pre-symptomatic phase of the disease [4, 5].
Mitochondria are intracellular organelles that generate adenosine 5-triphosphate (ATP), and mitochondrial dysfunction has been implicated in neurological and psychiatric disorders such as Huntington’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, bipolar disorder, major depressive disorder, and ASD [6-9]. It is known that defects in mitochondrial oxidative phosphorylation result in increased lactate and acyl-carnitine levels, abnormal lactate-to-pyruvate ratios, and accumulation of alanine in the plasma and urine [10]. There are a variety of candidate biomarkers associated with mitochondrial dysfunction, including lactate, pyruvate, carnitine, and alanine. Currently, there is a lack of reliable biochemical markers [11, 12]. Among the candidate biomarkers, lactate and pyruvate are the best known for having elevated levels in the plasma [10,13-15]. Since Lombard [16] proposed a link between ASD and mitochondrial dysfunction, many researchers have tried to identify mitochondria that might contribute to the pathogenesis of ASD, and there is accumulating evidence supporting their role in ASD [11,17-21]. One large population-based study in Portugal suggested that the prevalence of mitochondrial disease in ASD was approximately 7.2%; it also found that 20.3% of 69 patients had hyperlactacidemia, a biochemical marker of mitochondrial dysfunction [22]. In addition, Weissman et al. [17] suggested the term “mitochondrial autism” and provided biochemical evidence of mitochondrial dysfunction in the blood of 24/25 children with ASD. In their study, 76%, 53%, and 36% had elevated lactate, pyruvate, and alanine, respectively. In addition to lactate and pyruvate, mitochondrial DNA (mtDNA) is also a biological marker of mitochondria. Mitochondria contain their own mtDNA, which encodes essential subunits of the respiratory chain [23]. The mtDNA copy number has been suggested as a strong biomarker for mitochondrial dysfunction [24]. Our previous research found that ASD patients had higher relative mtDNA copy numbers than their unaffected siblings, and there was a relationship between mtDNA copy number and communication phenotype in a Korean population [25].
Recent studies involving biochemical markers of mitochondria have often been conducted on Caucasian populations, and studies on Asian populations are rare. Since it is not appropriate to apply these results to the Asian population, it is necessary to verify the results of research in foreign countries in a Korean population. Moreover, there has been no family comparison study that could control for environmental factors. Therefore, the objective of this study was to evaluate biochemical markers associated with mitochondrial function in patients with ASD and their unaffected family members who share a living environment in the Korean population.
MATERIALS AND METHODS
Participants
Participants with ASD, both of their biological parents, and their unaffected siblings were recruited through child and adolescent psychiatric clinics at Seoul National University Bundang Hospital. All ASD probands and their siblings were initially screened by two board-certified child psychiatrists based on the diagnostic criteria of the Diagnostic and Statistical Manual, 5th edition (DSM-5) [1] and through standardized diagnostic procedures using the Korean version of the Autism Diagnostic Observation Schedule (ADOS) [26] and the Autism Diagnostic Interview-Revised (ADI-R) [27]. To examine intelligence, we used the Korean Educational Development Institute-Wechsler Intelligence Scale for Children-Revised (KEDI-WISC-R) [28] for children with language and Korean-Leiter International Performance scale-Revised [29] for children without language. Social ability was assessed using the Social Communication Questionnaires (SCQ) [30] and the Social Responsiveness Scale second edition (SRS-2) [31]. We divided probands with ASD into the Affected Group (AG) and their unaffected family members (biological parents and unaffected siblings) into the Unaffected Group (UG). Any participant who had any neurological disease, serious medical condition, metabolic disease, or chromosomal anomaly, or a parent who declared that they had non-Korean ethnicity were excluded from the study. The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB no. B-1106/129-009) and written informed consent was obtained from the parents of all participants.
Measurements
Autism Diagnostic Observation Schedule (ADOS) [26]The ADOS is a standardized semi-structured test designed to diagnose ASD by observing communication and social behaviors during play and/or an interview. The ADOS has five modules (toddler, 1 to 4 modules). Each module comprises a different combination of activities and is selected according to the expressive language level and chronological age of the patient. It takes 35~40 minutes to administer. The ADOS is scored in five domains: language and communication, reciprocal social interaction, imagination, stereotyped behaviors and restricted interests, and other abnormal behaviors. The behaviors are coded from 0 (no evidence of abnormality) to 3 (markedly abnormal behavior).
Autism Diagnostic Interview-Revised (ADI-R) [27]The ADI-R is a semi-structured investigator-based interview for parents or primary caregivers. It consists of 93 items that assess the child’s communication; social development; play; and restricted, repetitive, and stereotyped behaviors that direct caregivers to reflect on the child’s early developmental history. The ADI-R is coded from 0 (socially appropriate level) to 3 (very severe) and consists of three diagnostic domains: social interactions, communication, and repetitive and stereotyped behaviors.
Social Communication Questionnaires (SCQ) [30]The SCQ consists of two forms, “Current” and “Lifetime,” which include 40 “yes or no” items rated by caregivers/parents of individuals aged 24 months or above. The items are extracted from the ADI-R, and the test can be implemented in less than 10 minutes. The SCQ assesses behaviors of an individual in three domains: 1) social interaction, 2) language and communication, and 3) restricted repetitive behavior.
Social Responsiveness Scale (SRS) [31]The SRS is used to screen children at risk of ASD and is answered by parents or caregivers. The SRS consists of measures regarding the child’s social interactions, communication, and stereotyped behaviors. The SRS-2 has four forms: school-age (age, 4~18 years), preschool (age, 2.5~4.5 years), adult (age, 19 years and older), and adult self-report. It has 65 questions, rated on a Likert scale from 1 (“not at all”) to 4 (“almost always”), to measure the severity of ASD.
Chemical markersLactate, pyruvate, and lactate-to-pyruvate ratio were examined in the peripheral blood of probands with ASD, and their biological parents and unaffected siblings using an enzymatic assay. For measurement, a Modular Analytics P (Roche, Germany) and Photometer A-6 (BENSRL, Italy) were used. Lactate ≥22 mg/dl, pyruvate ≥1.4 mg/dl, and lactate-to-pyruvate ratio >25 were considered abnormal. The clinical variables were compared in the subjects with higher (>25) and lower (≤25) lactate-to-pyruvate ratio within affected individuals.
mtDNA copy number analysis and methylation-specific PCR for the PPARGC1A gene promoter regionBlood samples from all participants were stored at -70°C in EDTA-coated tubes. Total DNA purification was performed using the G-spin Genomic DNA Extraction Kit (Intron, Daejeon, Korea). A Nanodrop 2000 spectrophotometer (Thermo Scientific, Korea) was used to calculate the quantity and quality of the DNA. The mtDNA copy number was evaluated based on the ratio of mtDNA to nuclear DNA, and experiments were performed according to a previous report [25]. In addition, to assess the DNA methylation ratio of the promoter region of the
Analyses
Statistical analyses were performed using SPSS Statistics 22 (IBM Corp., Armonk, NY, USA). Baseline characteristics were compared between the AG and UG using the chi-square test (χ2) for sex and the Student’s t-test for age. Differences were examined using paired t-tests for both groups, and the outcomes were compared, adjusting for age and sex using regression analysis. A chi-squared test was performed to determine the ratio of higher levels of chemical variables in the two groups. The relationship between biomarkers and clinical phenotype by ADOS and ADI-R was evaluated by performing correlation analysis. Statistical significance was defined as p<0.05.
RESULTS
A total of 59 subjects in the AG and 135 in the UG participated in the study. The AG included 57 ASD patients and two siblings who were diagnosed during screening. The UG included 57 fathers, 59 mothers, and 20 siblings. The mean age of the AG was 100.37±56.24 months old and that of the UG was 437.97±154.66 months (father: 509±73.42 months old, mother; 486±87.44 months old, sibling; 101±50.34 months old). Only 16.95% of the AG were female, while 52.21% of the UG were female; the sex ratio was statistically significantly different (χ2=19.22, p<0.01). The mean IQ in the AG as evaluated using the KEDI-WISC-R was 74.74±20.37 (Table 1).
The AG had a significantly higher lactate and lactate-to-pyruvate ratio than those in the UG (lactate 19.79±11.29 vs. 13.84±6.12, p<0.01, lactate-to-pyruvate ratio 21.47±18.43 vs. 15.03±9.37, p<0.05) (Table 2). Table 3 shows the difference in the frequency of subjects with abnormally high lactate levels, pyruvate levels, and lactate-to-pyruvate ratios. The AG had a significantly higher frequency of abnormally high lactate and lactate-to-pyruvate ratio than the UG (lactate 32.20% vs. 8.82%, lactate-to-pyruvate ratio 28.81% vs. 5.88%, p<0.01). However, there were no significant differences when the AG and siblings were analyzed separately.
The correlation between biomarkers and clinical phenotypes as identified using the ADOS and ADI-R was analyzed in the AG. The relationship between lactate levels and the repetitive behavior domain of the ADI-R was statistically significant (r=0.437, p<0.01; Pearson’s correlation, Table 4). However, there were no significant correlations between pyruvate, lactate-to-pyruvate ratio, mtDNA copy number, and clinical phenotypes.
To investigate the differences in chemical and clinical variables within the ASD group, the analysis was conducted in two groups, higher and lower lactate-to-pyruvate ratio. The lactate-to-pyruvate ratio is normally considered high when it is above 25. This ratio was used to divide subjects into high and low groups (high ratio, n=15; low ratio, n=43) and compare clinical and biochemical variables. As shown in Table 5, there was a significant difference in the pyruvate and lactate values between the two groups. Other clinical variables included severity of AD-related symptoms, cognitive skills and intelligence, age of the parent at the time of pregnancy, and clinically meaningful events (severe emesis, hemorrhage, thyroid abnormalities, and eclampsia) did not reveal significant differences between the two groups. In addition, no significant differences in genetic variables (mtDNA copy number variation and PGC-1 α promoter region methylation ratio) were found between the two groups.
DISCUSSION
This study investigated the biochemical markers associated with mitochondrial function in patients with ASD and their unaffected family members. The AG had a higher lactate level and lactate-to-pyruvate ratio than the UG, and the frequency of subjects with a higher lactate and lactate-to-pyruvate ratio was higher in the AG. In addition, there was a statistically significant relationship between lactate level and clinical phenotype for repetitive behavior in ASD.
Recently, several studies of genetics, biochemistry, and cellular mechanisms, such as calcium signaling and apoptosis, have been conducted that suggest a link between mitochondrial dysfunction and ASD [33]. This is the first study to explore mitochondria-related biomarkers by comparing subjects in the same family environment. These results support previous investigations showing that higher lactate levels and lactate-to-pyruvate ratios are biochemical markers of ASD. Elevated lactate was reported to be the first indicator of mitochondrial disorder in ASD by Coleman in 1985 [34]. Since then, it has been reported to be a potential biomarker for abnormal mitochondrial metabolism in children with ASD [13, 35, 36]. Pyruvate and the lactate-to-pyruvate ratio have also been mentioned as candidate biomarkers of ASD [35, 37]. Four previous studies with sample sizes ranging from 30 to 210 individuals have reported a prevalence of elevated lactate and pyruvate levels in ASD ranging between 17.2% and 40% [13, 22, 38, 39]. A recent study of potential biological diagnostic markers with 41 ASD patients and 41 non-ASD controls confirmed previous results regarding the relationship between mitochondrial dysfunction and ASD with pyruvate, creatine kinase, complex 1, cascade 7, and glutathione. Furthermore, they also found abnormalities in lactate dehydrogenase (LDH) in children with ASD [35]. While there have been many findings supporting the association of mitochondrial dysfunction and ASD, it is not clear how mitochondrial dysfunction is related to the development or pathogenesis of ASD [11]. However, it is not surprising that mitochondrial dysfunction may lead to or cause neurodevelopmental disorders, including ASD, because mitochondria are the organelles responsible for aerobic energy production and developing neurons in the CNS depend on oxidative phosphorylation for critical developmental processes [40]. In addition, a postmortem study suggested that mitochondrial dysfunction may contribute to the vulnerability of developing autism [41]. Another way to evaluate the function of mitochondria indirectly is to measure mtDNA copy numbers. The mtDNA copy number is considered a marker of mitochondrial energy function because the mtDNA copy number is maintained at high levels in cells with high energy consumption. In other words, mtDNA copy number may increase in a compensatory mechanism for mitochondrial dysfunction [42-44].
To date, few studies have identified a quantitative relationship between the level of chemical markers and symptomatic severity of ASD. Our previous study comparing children with ASD and unaffected sibling pairs revealed a negative correlation between mtDNA copy number and the language and communication domain of the ADOS [25]. We found a positive correlation between the repetitive behavior domain of the ADI-R and lactate in ASD patients. Repetitive behavior is a core symptom of ASD. To our knowledge, this study is the first to show the link between lactate level and ASD phenotype. Therefore, it is difficult to determine the mechanism of mitochondrial dysfunction and the relationship between higher lactate levels and the clinical features of ASD. Considering that ASD is a complex trait, probably with a complex etiology, it might be essential to find biological markers tightly linked to clinical variables or subdomain symptoms of ASD. However, there have been few studies exploring biomarkers and specific clinical endpoints in ASD. Further studies are needed to determine the relationship between chemical and genetic markers and clinical symptoms of particular domains in ASD. Quantitative correlations of clinical symptom severity and markers of mitochondrial dysfunction have been replicated in other neuropsychiatric conditions, such as bipolar disorder, schizophrenia, major depressive disorder (MDD), migraine, and epilepsy. For example, one study showed a negative relationship between mtDNA copy number and psychomotor agitation and somatic symptoms in 118 patients with MDD and 116 healthy controls [8]. Higher lactate levels and poorer general cognitive function and functional capacity in schizophrenia have been reported, with increased anaerobic glycolysis caused by mitochondrial dysfunction suggested to be the cause of the increase in lactate levels in schizophrenia [45]. However, the exact mechanism remains unknown, and the direction of the reported changes has been inconsistent. Further studies are needed to evaluate the complex interplay of mtDNA, a chemical marker, and the development of clinical phenotypes [9, 46, 47].
mtDNA continues to be used as a biomarker to evaluate mitochondrial dysfunction and some studies have already found a correlation between mtDNA copy number and ASD [25, 48]. We found a higher mtDNA copy number in patients with ASD than in unaffected siblings in our previous study, which compared with 100 patients and siblings [25]. PGC-1α is considered to be a regulatory component for communication between mitochondrial biogenesis and control of fatty acid β-oxidation and tricyclic acid cycle enzyme expression; it is also highly expressed in cells with high ATP consumption [49]. In addition, it has been reported that the mtDNA mutator prematurely aging mice show increased LDH activity, which causes high brain lactate levels [50]. Therefore, it was hypothesized in this study that mtDNA copy number and PGC-1α regulate mitochondrial metabolites via epigenetic regulation. mtDNA copy number may be influenced by several factors, such as environmental factors, nuclear genetic backgrounds, and mtDNA heteroplasmy in different tissues [51, 52]. However, many studies have been conducted without controlling for environmental factors [48]. To compensate for this limitation, we used ASD patients and unaffected family members who share living environments and have the same genetic background because mtDNA is inherited maternally; although mtDNA is inherited from the same mother, the level of mitochondrial heteroplasmy of offspring is very different [53]. In other words, we hypothesized that increased lactate may be associated with epigenetic changes, such as DNA methylation, leading to changes in mtDNA in this study. However, there were no statistically significant differences in mtDNA copy number or PGC-1α promoter methylation levels between the AG and UG. Further analysis is needed in the future, taking into account different types of markers and clinical variables.
Many factors might affect mitochondrial metabolism, including age and environment such as diet, obesity, intrauterine malnutrition, and environmental pollutants [54]. However, it is not clear which factor predominates in the regulation of pyruvate and lactate metabolism. Therefore, one of the limitations of our study is that we could not control age of both group, while controlling other possible factors by using subjects from shared environment. Further investigation should be performed whether shared living environment on the mitochondria-related metabolites could override possible the effects of age.
Other limitations of current study are; first, the number of participants was relatively small, although the sample size provided adequate statistical power for the discovery of effects. Second, the age and sex of the UG were not matched with those of the AG because family members that were unaffected by ASD were used as controls. Age and sex are potential confounding factors that can affect biochemical markers. Third, lactate levels could be elevated for a variety of reasons, such as excessive muscle movement and long duration of tourniquet use. Although we used a tourniquet, we tried to use it for a short period of time to collect blood samples, and we tried to minimize the movement of participants; however, it still is a limitation as there was no correction for any differences. Currently, this is a major concern for researchers conducting similar metabolic studies.
In conclusion, to our knowledge, the present study is the first Korean population-based study in which the results suggest that biochemical markers related to mitochondrial dysfunction, especially a higher lactate level and lactate-to-pyruvate ratio, might be associated with the pathophysiology of ASD. In addition, this study has the advantage that it compared family members who share a living environment. Further larger studies using unrelated individuals are needed to control for the possible effects of age and sex on chemical biomarkers.
ACKNOWLEDGEMENTS
This work was supported by the disease-focused Healthcare Technology R&D project by the Ministry of Health and Welfare, Republic of Korea (HI14C2336), the Original Technology Research Program for Brain Science of the NRF funded by the Korean government, MSIT (NRF-2017M3C7A1027467) and MOE (NRF-2017R1D1A3B03033533).
Tables
Clinical data of samples
| Affected group (n=59) | Unaffected group (n=136) | ||||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (months) | Total | 100.37 | 56.24 | 437.97 | 154.66 |
| Father (n=57) | 509 | 73.42 | |||
| Mother (n=59) | 486 | 57.44 | |||
| Siblings (n=20) | 101 | 50.34 | |||
| Sex (female %) | Total | 16.95 | 52.21 | ||
| Siblings | 55 | ||||
| ADOS | Communication | 5.37 | 1.90 | 1.25 | 1.25 |
| Social interaction | 9.54 | 2.39 | 2.05 | 1.76 | |
| Play | 1.90 | 1.11 | 0.90 | 0.55 | |
| Repetitive behavior | 1.24 | 1.33 | 0.10 | 0.31 | |
| ADIR | Social interaction | 18.58 | 6.33 | 3.45 | 4.35 |
| Communication: verbal | 14.57 | 5.16 | 1.75 | 2.79 | |
| Communication: nonverbal | 9.32 | 3.52 | 1.10 | 2.15 | |
| Repetitive behavior | 4.41 | 2.63 | 0.50 | 1.19 | |
| KEDI-WISC-R | 74.74 | 20.37 | 100.72 | 15.53 | |
| K-Leiter-R | 72.32 | 16.12 | 44.11 | 40.77 | |
| SCQ | 16.67 | 8.50 | 3.80 | 3.81 | |
| SRS | 87.90 | 28.98 | 30.35 | 19.43 | |
ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; KEDI-WISC-R, Korean Educational Development Institute-Wechsler Intelligence Scale for Children-Revised; K-Leiter-R, Korean-Leiter International Performance scale - Revised; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale.
Differences in variables in affected and unaffected individuals
| Biomarkers | Group | Paired t-test | ||||
|---|---|---|---|---|---|---|
| Mean | SD | t | df | p value | ||
| Lactate | Affected group | 19.79 | 11.29 | -3.71 | 73.2 | 0.0003** |
| Unaffected group | 13.84 | 6.12 | ||||
| Pyruvate | Affected group | 1.10 | 0.45 | -1.45 | 193 | 0.1495 |
| Unaffected group | 1.01 | 0.37 | ||||
| Lactate-to-pyruvate ratio | Affected group | 21.47 | 18.43 | -2.55 | 71.35 | 0.0131* |
| Unaffected group | 15.03 | 9.37 | ||||
| mtDNA CNV | Affected group | 163.66 | 42.46 | 1.46 | 193 | 0.1466 |
| Unaffected group | 179.34 | 77.66 | ||||
| PGC-1α | Affected group | 0.17 | 0.17 | -0.55 | 178 | 0.5867 |
| Unaffected group | 0.16 | 0.09 | ||||
*p<0.05, **p<0.01.
mtDNA CNV, mitochondrial DNA copy number variation; PGC-1α, peroxisome proliferator-activated receptor gamma coactivator 1-alpha methylation ratio.
Frequency of higher level of markers in the two groups
| Affected group (n=59) | Unaffected group (n=136) | χ2 | df | p | |
|---|---|---|---|---|---|
| n (%) | n (%) | ||||
| Lactate ≥22 mg/dl | 19 (32.20) | 12 (8.82) | 16.12 | 1 | 0.0002** |
| Pyruvate ≥1.4 mg/dl | 11 (18.64) | 12 (8.82) | 3.56 | 1 | 0.0591 |
| Lactate-to-pyruvate ratio >25 | 17 (28.81) | 8 (5.88) | 18.66 | 1 | 0.0001** |
*p<0.05, **p<0.01.
Correlation between lactate and clinical variables in the affected group
| Lactate | ADOS | ADI-R | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Communication | Social interaction | Play | Repetitive behavior | Social interaction | Communication verbal | Communication nonverbal | Repetitive behavior | |||
| Lactate | 1 | |||||||||
| ADOS | Communication | 0.246 | 1 | |||||||
| Social interaction | 0.092 | 0.585** | 1 | |||||||
| Play | 0.069 | 0.182 | 0.190 | 1 | ||||||
| Repetitive behavior | 0.108 | 0.366** | 0.371** | 0.332* | 1 | |||||
| ADIR | Social interaction | 0.242 | 0.284* | 0.450** | 0.286* | 0.092 | 1 | |||
| Communication verbal | 0.147 | 0.332* | 0.425** | 0.256 | 0.019 | 0.778** | 1 | |||
| Communication nonverbal | 0.102 | 0.250 | 0.346** | 0.384** | 0.142 | 0.752** | 0.929** | 1 | ||
| Repetitive behavior | 0.437** | 0.168 | 0.212 | -0.014 | 0.096 | 0.408** | 0.305* | 0.229 | 1 | |
*p<0.05, **p<0.01.
ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule.
Differences in clinical and chemical variables in subjects with higher and lower lactate-to-pyruvate ratios in the affected group
| Higher ratio (>25) (n=16) | Lower ratio (≤25) (n=43) | t | df | p | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Lactate | 28.47 | 15.96 | 16.56 | 6.77 | -2.89 | 17.05 | 0.0102* | |
| Pyruvate | 0.83 | 0.47 | 1.20 | 0.41 | 2.91 | 57.00 | 0.0052** | |
| Lactate-to-pyruvate ratio | 40.92 | 26.51 | 14.23 | 4.51 | -4.01 | 15.32 | 0.0011** | |
| ADI-R | Social interaction | 20.50 | 4.23 | 17.86 | 6.86 | 0.07 | 57.00 | 0.1564 |
| Communication: verbal | 15.50 | 3.23 | 14.22 | 5.73 | -0.73 | 42.00 | 0.4701 | |
| Communication: nonverbal | 10.13 | 2.68 | 9.02 | 3.77 | 0.20 | 57.00 | 0.2891 | |
| Repetitive behavior | 6.56 | 3.20 | 5.19 | 2.88 | -1.58 | 57.00 | 0.1189 | |
| ADOS | Communication | 6.13 | 1.78 | 5.09 | 1.89 | -1.89 | 57.00 | 0.0633 |
| Social interaction | 9.81 | 1.68 | 9.44 | 2.61 | -0.53 | 57.00 | 0.6004 | |
| Play | 1.81 | 1.11 | 1.93 | 1.12 | 0.36 | 57.00 | 0.7204 | |
| Repetitive behavior | 1.06 | 1.00 | 1.30 | 1.44 | 0.61 | 57.00 | 0.5428 | |
| KEDI-WISC-R | 73.33 | 23.77 | 75.12 | 19.74 | 0.23 | 40.00 | 0.8187 | |
| K-Leiter-R | 69.17 | 18.54 | 73.77 | 15.48 | 0.57 | 17.00 | 0.5779 | |
| SCQ | 16.88 | 6.20 | 16.58 | 9.37 | -0.12 | 52.00 | 0.9083 | |
| SRS | 87.06 | 19.73 | 88.21 | 32.01 | 0.13 | 56.00 | 0.8938 | |
| Paternal age | 31.94 | 3.974 | 32.63 | 6.091 | 0.42 | 57.00 | 0.6762 | |
| Maternal age | 33.81 | 3.885 | 34.98 | 6.585 | 0.66 | 57.00 | 0.5198 | |
| Prenatal events (%) | 10 (62.50) | 17 (39.53) | χ2=2.47 | 1 | 0.1153 | |||
| Perinatal events (%) | 6 (37.50) | 11 (25.58) | χ2=0.81 | 1 | 0.3694 | |||
| mtDNA CNV | 162.50 | 44.05 | 164.09 | 42.38 | 0.13 | 57.00 | 0.8991 | |
| PGC-1α | 0.15 | 0.07 | 0.17 | 0.20 | 0.50 | 52.00 | 0.6210 | |
*p<0.05, **p<0.01.
ADI-R, Autism Diagnostic Interview-Revised; ADOS, Autism Diagnostic Observation Schedule; KEDI-WISC-R, Korean Educational Development Institute-Wechsler Intelligence Scale for Children-Revised; K-Leiter-R, Korean-Leiter International Performance scale - Revised; mtDNA CNV, mitochondrial DNA copy number variation; PGC-1α, peroxisome proliferator-activated receptor gamma coactivator 1-alpha methylation ratio; SCQ, Social Communication Questionnaire; SRS, Social Responsiveness Scale.
References
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5, 5th ed. American Psychiatric Publishing, Washington, D.C
- Duchan E, Patel DR (2012) Epidemiology of autism spectrum disorders. Pediatr Clin North Am 59: 27-43, ix-x
- Xu G, Strathearn L, Liu B, Bao W (2018) Prevalence of autism spectrum disorder among US children and adolescents, 2014-2016. JAMA 319: 81-82
- Goldani AA, Downs SR, Widjaja F, Lawton B, Hendren RL (2014) Biomarkers in autism. Front Psychiatry 5: 100
- Howsmon DP, Kruger U, Melnyk S, James SJ, Hahn J (2017) Classification and adaptive behavior prediction of children with autism spectrum disorder based upon multivariate data analysis of markers of oxidative stress and DNA methylation. PLoS Comput Biol 13: e1005385
- Trushina E, McMurray CT (2007) Oxidative stress and mitochondrial dysfunction in neurodegenerative diseases. Neuroscience 145: 1233-1248
- Martin LJ (2006) Mitochondriopathy in Parkinson disease and amyotrophic lateral sclerosis. J Neuropathol Exp Neurol 65: 1103-1110
- Chung JK, Lee SY, Park M, Joo EJ, Kim SA (2019) Investigation of mitochondrial DNA copy number in patients with major depressive disorder. Psychiatry Res 282: 112616
- Kuang H, Duong A, Jeong H, Zachos K, Andreazza AC (2018) Lactate in bipolar disorder: a systematic review and meta-analysis. Psychiatry Clin Neurosci 72: 546-555
- Haas RH (2010) Autism and mitochondrial disease. Dev Disabil Res Rev 16: 144-153
- Rossignol DA, Frye RE (2012) Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry 17: 290-314
- Haas RH, Parikh S, Falk MJ, Saneto RP, Wolf NI, Darin N, Cohen BH (2007) Mitochondrial disease: a practical approach for primary care physicians. Pediatrics 120: 1326-1333
- László A, Horváth E, Eck E, Fekete M (1994) Serum serotonin, lactate and pyruvate levels in infantile autistic children. Clin Chim Acta 229: 205-207
- Chugani DC, Sundram BS, Behen M, Lee ML, Moore GJ (1999) Evidence of altered energy metabolism in autistic children. Prog Neuropsychopharmacol Biol Psychiatry 23: 635-641
- Frye RE, Rossignol DA (2011) Mitochondrial dysfunction can connect the diverse medical symptoms associated with autism spectrum disorders. Pediatr Res 69(5 Pt 2): 41R-47R
- Lombard J (1998) Autism: a mitochondrial disorder? . Med Hypotheses 50: 497-500
- Weissman JR, Kelley RI, Bauman ML, Cohen BH, Murray KF, Mitchell RL, Kern RL, Natowicz MR (2008) Mitochondrial disease in autism spectrum disorder patients: a cohort analysis. PLoS One 3: e3815
- Palmieri L, Persico AM (2010) Mitochondrial dysfunction in autism spectrum disorders: cause or effect? . Biochim Biophys Acta 1797: 1130-1137
- Anderson MP, Hooker BS, Herbert MR (2008) Bridging from cells to cognition in autism pathophysiology: biological pathways to defective brain function and plasticity. Am J Biochem Biotechnol 4: 167-176
- Anitha A, Nakamura K, Thanseem I, Yamada K, Iwayama Y, Toyota T, Matsuzaki H, Miyachi T, Yamada S, Tsujii M, Tsuchiya KJ, Matsumoto K, Iwata Y, Suzuki K, Ichikawa H, Sugiyama T, Yoshikawa T, Mori N (2012) Brain region-specific altered expression and association of mitochondria-related genes in autism. Mol Autism 3: 12
- Goh S, Dong Z, Zhang Y, DiMauro S, Peterson BS (2014) Mitochondrial dysfunction as a neurobiological subtype of autism spectrum disorder: evidence from brain imaging. JAMA Psychiatry 71: 665-671
- Oliveira G, Diogo L, Grazina M, Garcia P, Ataíde A, Marques C, Miguel T, Borges L, Vicente AM, Oliveira CR (2005) Mitochondrial dysfunction in autism spectrum disorders: a population-based study. Dev Med Child Neurol 47: 185-189
- Picard M, McEwen BS (2014) Mitochondria impact brain function and cognition. Proc Natl Acad Sci U S A 111: 7-8
- Gu F, Chauhan V, Kaur K, Brown WT, LaFauci G, Wegiel J, Chauhan A (2013) Alterations in mitochondrial DNA copy number and the activities of electron transport chain complexes and pyruvate dehydrogenase in the frontal cortex from subjects with autism. Transl Psychiatry 3: e299
- Yoo HJ, Park M, Kim SA (2017) Difference in mitochondrial DNA copy number in peripheral blood cells between probands with autism spectrum disorders and their unaffected siblings. World J Biol Psychiatry 18: 151-156
- Lord C, Rutter M, DiLavore PC, Risi S (2008) Autism diagnostic observation schedule: ADOS manual, Western Psychological Services, Los Angeles, CA
- Lord C, Rutter M, Le Couteur A (1994) Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 24: 659-685
- Park K, Yoon J, Park H, Park H, Kwon K (1986) Development of KEDI-WISC, individual intelligence test for Korean children, Korean Educational Development Institute, Seoul
- Shin M, Cho S (2010) Korean Leiter international performance scale-revised (K-Leiter-R), Hakjisa, Seoul
- Rutter M, Bailey A, Lord C (2003) The social communication questionnaire: manual, Western Psychological Services, Los Angeles, CA
- Constantino JN, Gruber CP (2012) Social responsiveness scale: SRS-2 software kit, 2nd ed. Western Psychological Services, Torrane, CA
- Kim JI, Lee SY, Park M, Kim SY, Kim JW, Kim SA, Kim BN (2019) Peripheral mitochondrial DNA copy number is increased in Korean attention-deficit hyperactivity disorder patients. Front Psychiatry 10: 506
- Griffiths KK, Levy RJ (2017) Evidence of mitochondrial dysfunction in autism: biochemical links, genetic-based associations, and non-energy-related mechanisms. Oxid Med Cell Longev 2017: 4314025
- Coleman M, Blass JP (1985) Autism and lactic acidosis. J Autism Dev Disord 15: 1-8
- Khemakhem AM, Frye RE, El-Ansary A, Al-Ayadhi L, Bacha AB (2017) Novel biomarkers of metabolic dysfunction is autism spectrum disorder: potential for biological diagnostic markers. Metab Brain Dis 32: 1983-1997
- Shahjadi S, Khan AS, Ahmed MU (2017) Mitochondrial dysfunction in early diagnosed autism spectrum disorder children. J Dhaka Med Coll 26: 43-47
- Essa MM, Guillemin GJ, Waly MI, Al-Sharbati MM, Al-Farsi YM, Hakkim FL, Ali A, Al-Shafaee MS (2012) Increased markers of oxidative stress in autistic children of the Sultanate of Oman. Biol Trace Elem Res 147: 25-27
- Moreno H, Borjas L, Arrieta A, Sáez L, Prassad A, Estévez J, Bonilla E (1992) [Clinical heterogeneity of the autistic syndrome: a study of 60 families]. Invest Clin 33: 13-31. Spanish
- Correia C, Coutinho AM, Diogo L, Grazina M, Marques C, Miguel T, Ataíde A, Almeida J, Borges L, Oliveira C, Oliveira G, Vicente AM (2006) Brief report: high frequency of biochemical markers for mitochondrial dysfunction in autism: no association with the mitochondrial aspartate/glutamate carrier SLC25A12 gene. J Autism Dev Disord 36: 1137-1140
- Valenti D, de Bari L, De Filippis B, Henrion-Caude A, Vacca RA (2014) Mitochondrial dysfunction as a central actor in intellectual disability-related diseases: an overview of Down syndrome, autism, Fragile X and Rett syndrome. Neurosci Biobehav Rev 46(Pt 2): 202-217
- Chauhan A, Gu F, Essa MM, Wegiel J, Kaur K, Brown WT, Chauhan V (2011) Brain region-specific deficit in mitochondrial electron transport chain complexes in children with autism. J Neurochem 117: 209-220
- Moyes CD, Battersby BJ, Leary SC (1998) Regulation of muscle mitochondrial design. J Exp Biol 201(Pt 3): 299-307
- Clay Montier LL, Deng JJ, Bai Y (2009) Number matters: control of mammalian mitochondrial DNA copy number. J Genet Genomics 36: 125-131
- Lee HC, Wei YH (2005) Mitochondrial biogenesis and mitochondrial DNA maintenance of mammalian cells under oxidative stress. Int J Biochem Cell Biol 37: 822-834
- Rowland LM, Pradhan S, Korenic S, Wijtenburg SA, Hong LE, Edden RA, Barker PB (2016) Elevated brain lactate in schizophrenia: a 7 T magnetic resonance spectroscopy study. Transl Psychiatry 6: e967
- Khurana DS, Valencia I, Goldenthal MJ, Legido A (2013) Mitochondrial dysfunction in epilepsy. Semin Pediatr Neurol 20: 176-187
- Yorns WR Jr, Hardison HH (2013) Mitochondrial dysfunction in migraine. Semin Pediatr Neurol 20: 188-193
- Giulivi C, Zhang YF, Omanska-Klusek A, Ross-Inta C, Wong S, Hertz-Picciotto I, Tassone F, Pessah IN (2010) Mitochondrial dysfunction in autism. JAMA 304: 2389-2396
- Lehman JJ, Barger PM, Kovacs A, Saffitz JE, Medeiros DM, Kelly DP (2000) Peroxisome proliferator-activated receptor gamma coactivator-1 promotes cardiac mitochondrial biogenesis. J Clin Invest 106: 847-856
- Ross JM, Öberg J, Brené S, Coppotelli G, Terzioglu M, Pernold K, Goiny M, Sitnikov R, Kehr J, Trifunovic A, Larsson NG, Hoffer BJ, Olson L (2010) High brain lactate is a hallmark of aging and caused by a shift in the lactate dehydrogenase A/B ratio. Proc Natl Acad Sci U S A 107: 20087-20092
- Hao H, Morrison LE, Moraes CT (1999) Suppression of a mitochondrial tRNA gene mutation phenotype associated with changes in the nuclear background. Hum Mol Genet 8: 1117-1124
- Betts J, Jaros E, Perry RH, Schaefer AM, Taylor RW, Abdel-All Z, Lightowlers RN, Turnbull DM (2006) Molecular neuropathology of MELAS: level of heteroplasmy in individual neurones and evidence of extensive vascular involvement. Neuropathol Appl Neurobiol 32: 359-373
- Giles RE, Blanc H, Cann HM, Wallace DC (1980) Maternal inheritance of human mitochondrial DNA. Proc Natl Acad Sci U S A 77: 6715-6719
- Hollinshead KE, Tennant DA (2016) Mitochondrial metabolic remodeling in response to genetic and environmental perturbations. Wiley Interdiscip Rev Syst Biol Med 8: 272-285





