Articles
Article Tools
Stats or Metrics
Article
Short Communication
Exp Neurobiol 2022; 31(5): 343-352
Published online October 31, 2022
https://doi.org/10.5607/en22030
© The Korean Society for Brain and Neural Sciences
The Association of White Matter Tracts with Alexithymia among Individuals with Major Depressive Disorder
Youbin Kang1, Aram Kim1, Wooyoung Kang1, Kyu-Man Han2 and Byoungjoo Ham2*
1Department of Biomedical Sciences, Korea University College of Medicine, Seoul 02841,
2Department of Psychiatry, Korea University Anam Hospital, Korea University College of Medicine, Seoul 02841, Korea
Correspondence to: *To whom correspondence should be addressed.
TEL: 82-2-2920-6843, FAX: 82-2-2927-2836
e-mail: hambj@korea.ac.kr
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Alexithymia is characterized by impairments in the processing of emotions. Although the disruptions in the white matter (WM) integrity in Major depressive disorder (MDD) has frequently been reported, the underlying relationship with alexithymia remains unclear. In the present study, we investigated WM tracts with Tracts Constrained by UnderLying Anatomy approach to discover potential associations between alexithymia and WM integrity to identify the neural basis of impaired emotional self-awareness in MDD. 101 patients with MDD and 99 healthy sex- and age-matched individuals underwent diffusion-weighted imaging. All participants were assessed with the 20-item Toronto Alexithymia Scale (TAS). TAS scores were significantly higher in MDD patients than in controls. Patients with MDD exhibited significantly lower FA values in the left inferior longitudinal fasciculus and it also showed negative associations with TAS. These results contribute to the neurobiological evidence on the association between MDD and alexithymia. Additionally, they suggest that reduced white matter integrity in the regions constitutes a principal pathophysiology underlying impaired emotional recognition and description in MDD.
Graphical Abstract
Keywords: Alexithymia, TAS-20, White matter, Inferior longitudinal fasciculus, Superior longitudinal fasciculus, Probabilistic tractography
INTRODUCTION
Major depressive disorder (MDD), a major public health concern, is a common psychiatric illness with the current prevalence of 6.0% [1]. Alexithymia was first introduced by Sifneos [2] to describe the discrepancy in the processing of emotions characterized by struggles in recognizing and communicating one’s feelings, restriction of emotional expressions and imaginations, and a thinking style preoccupied by external events and limited introspections [3-5]. The Toronto Alexithymia Scale (TAS) includes three subscales, namely, difficulties in identifying feelings (DIF), difficulties in describing feelings (DDF), and externally oriented thinking (EOT) [6] and the total score of over 61 is considered to be alexithymic. There is still an ongoing debate on whether alexithymia is a stable personality trait or a state-dependent phenomenon. However, it’s role in the onset of psychiatric disorder, MDD in particular is undeniable.
Studies have not only reported higher prevalence of alexithymia in MDD patients [7-9], but have also identified aggravated depressive symptoms in people with alexithymia [4, 7]. Despite such solid relationships proposed between alexithymic traits and MDD, the association between neural activity in response to alexithymia remains to be defined as alexithymia is a multi-dimensional paradigm with both cognitive and affective characteristics [10].
Damages in the corpus-callosum (CC) leading to the cognitive characteristics of alexithymia with the disturbed interhemispheric transferal of information is one of the most prominent view in neural perspective [11-13]. Recent studies have focused on brain structures such as the insula and the anterior cingulate cortex (ACC) in relation with alexithymia. A PET study comparing TAS scores and its association with visceral stimulation [14] have identified increased cerebral blood flows in the insula during colonic distension and increased activity in the ACC during physical stimulation. The increase in neural activity in the insula is also supported by a number of functional studies [15-17] reporting association with hyperawareness of somatosensory signals in alexithymia. Others, conversely, have reported negative correlations with alexithymia suggesting reductions in attention and response selection [18, 19]. Grabe et al. have identified structural alterations of the brain including reductions in volume in the dorsal anterior cingulate cortex, left inferior temporal gyrus, cerebellum, fusiform gyrus, and inferior temporal gyrus in the patients [20]. Moreover, a diffusion MRI connectometry study have reported significant correlation between TAS scores and increased microstructural connectivity in the body of corpus callosum, bilateral fornix, left arcuate fasciculus, corticospinal and cingulum tracts [21].
Despite such efforts in revealing the underlying neural correlates in alexithymia in MDD, the exact underpinning mechanisms remain unclear and there is no sufficient data on the white matter (WM) changes evidenced in alexithymia. Only a recent study has reported negative correlation between white-matter integrity of CC, left superior longitudinal fasciculus (SLF), and the inferior longitudinal fasciculus (ILF) in schizophrenia [22]. Previous studies have recognized significantly lower FA values of the forceps major of the corpus callosum and left ILF, AD values of the left SLF, and of parahippocampal cingulum in patients with MDD compared to healthy individuals [23, 24].
Therefore, in the present study, we aimed to examine the white-matter connectivity in a group of patients diagnosed with MDD, and a matched group of healthy individuals using TRActs Constrained by UnderLying Anatomy (TRACULA) method. Sensitive to specifically targeted white matter tract, it allows the identification of the specific tracts with white matter alterations [25]. By running a whole-brain tractography in the native diffusion space, it reconstructs the 18 major white matter fibers and models the likelihood of the anatomical neighborhood. The method also implements both ball-and-stick model and global tractography enabling the estimation of areas of low anisotropy and tract crossing [26]. We also aimed to explore the relationship between alexithymia and depression. We hypothesized that MDD patients would display altered integrity in white matter (WM) tracts and especially those related to cortico-limbic circuit alterations. Furthermore, we also hypothesized that alexithymia would be associated with certain white matter tracts alterations especially in the CC, ILF, and SLF.
MATERIALS AND METHODS
Participants
A total of 101 patients with MDD (54 females and 47 males) and 99 healthy controls (HCs) (63 females and 36 males) were included in the present study. All participants were diagnosed with MDD by two board-certified psychiatrists (B.-J. Ham and K.-M. Han) using the Structured Clinical Interview from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision Axis I disorders (SCID). The severity of depressive symptoms was assessed using the 17-item Hamilton Depression Rating Scale (HDRS) [27]. All clinical scales were assessed at the time of the MRI scanning. The exclusion criteria were: (i) comorbidity with any other major psychiatric disorder(s); (ii) psychotic features, such as delusions or hallucinations; (iii) history of a serious or uncontrolled medical illness; (iv) history of primary neurological illness; (v) any contraindication to MRI scanning, such as metal implants or claustrophobia. 99 HCs aging from 19~65 were recruited from the community using advertisement and were assessed by two psychiatrists using the same exclusion criteria used for MDD patients. Informed consent was obtained from all participants for their participation after a thorough explanation of the study. The study protocol was approved by the Institutional Review Board (IRB) or Korea University Anam Hospital (2015AN009) and was in accordance with the approved principles of the Declaration of Helsinki.
Measurement of alexithymia
To assess alexithymia in participants, self-reporting questionnaires of TAS [28] were used. The scale is further categorized in three subscales including difficulty describing feelings (DDF), difficulty identifying emotion (DIF), and externally-oriented thinking (EOT). Items are rated using a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree) and high TAS scores indicate high alexithymic traits of having more hardships in describing or identifying emotions.
MRI data acquisition
Three dimensional structural MRI scans were acquired using a 3.0-Tesla TrioTM whole-body imaging system (Siemens Healthcare GmbH, Erlangen, Germany) at the Korea University MRI Center using a dedicated 32-channel high-resolution phased-array coil for brain imaging. Diffusion-weighted MR images were acquired using an echo-planar imaging with the following parameters: repetition time, 7,000 ms; echo time, 86 ms; field of view, 224 mm; matrix size, 112×112; orientation, transverse; number of diffusion directions, 64; voxel size, 1.8×1.8×3.0 mm3; number of B0 images, 1; number of slices, 56; b-values, 0 and 600 s/mm2; acceleration factor [GRAPPA], 2 with 34 reference lines for the phase encoding direction and a 6/8-phase partial Fourier.
Image processing
The DTIs of all participants were processed using the probabilistic tractography functions in TRACULA (Tracts Constrained by UnderLying Anatomy) implemented in the Freesurfer 5.3 development version (Laboratory for Computational Neuroimaging, Athinoula A. Martinos Center for Biomedical Imaging, Charlestown, MA, USA; http://surfer.nmr.mgh.harvard.edu). Combined with previously attained information regarding the likelihood of each white matter tract to pass through or next to each cortical parcellation and subcortical segmentation analyzed in the FreeSurfer, the algorithm reconstructs 18 major white matter tracts with a “ball-and-stick” model of local diffusion orientations to estimate the probabilistic distribution preserving the individual variation in WM tracts and assuring selection of the same white matter tract in each participant. The 18 major tracts include: the forceps major and minor of the corpus callosum, the anterior thalamic radation (ATR), cingulum – angular bundle (CAB), cingulum – cingulate gyrus endings (CCG), corticospinal tract (CST), inferior longitudinal fasciculus (ILF), superior longitudinal fasciculus – parietal endings (SLFP), superior longitudinal fasciculus – temporal endings (SLFT), and uncinate fasciculus (UF). Additionally, the DTI parameters of fractional anisotropy (FA), axial diffusivity (AD), radial diffusivity (RD), and mean diffusivity (MD) were extracted.
Statistical analyses
Statistical analyses were performed using SPSS Statistics, Version 25.0 (IBM Corp., Armonk, NY, USA). One-way analysis of covariance (ANCOVA) was performed to calculate the differences in DTI scalar values (FA, AD, RD, and MD) for the 18 major WM tracts between patients with MDD and HCs. We included age, sex, and education level as nuisance covariates to prevent potential confounding effects. For multiple comparisons, we applied Bonferroni correction for the 4 scalars and 18 tracts to the analysis (p<0.05/72=0.00069).
A 2-tailed Pearson correlation was executed to analyze the correlations between TAS, depression severity and DTI scalar values, controlling for age, gender, and TICV. To correct for multiple comparisons, Bonferroni correction was applied for the 4 scalars, 1 tract of interest, and 5 measures (p<0.05/20=0.0025).
In the secondary analysis, we investigated the potential association between severity of depressive symptoms and TAS within MDD group using a Pearson’s partial correlation analysis between TAS and its subcategories and individual scores of HDRS with covariates of age and gender. Bonferroni correction was also applied to correct for multiple comparison (p<0.05/68=0.00074). To further assess the influence of severity of depression, we also have analyzed the difference in DTI scalar values with depression severity as an additional covariate. Bonferroni correction for the 4 scalars and 18 tracts was applied to the analysis (p<0.05/72=0.00069).
To analyze the sociodemographic and clinical differences between the groups, independent t-test was implemented to analyzed age, education level, HDRS score, and TICV and the chi-square test to analyze the difference of sex distribution.
RESULTS
Demographic and clinical characteristics
The demographic characteristics of each participant, including age, sex, education level, and the clinical characteristics, such as the self-questionnaires (HDRS and TAS) are summarized in Table 1. No significant differences were observed in the demographic variables tested between MDD patients and HCs. A significant difference was present for HDRS between the diagnostic groups, with the MDD group showing higher HDRS scores compared to HCs (p<0.001). TAS scores, including the subscales, also differed significantly between the two groups (p<0.001).
Groups comparison of WM integrity between patients with MDD and HCs
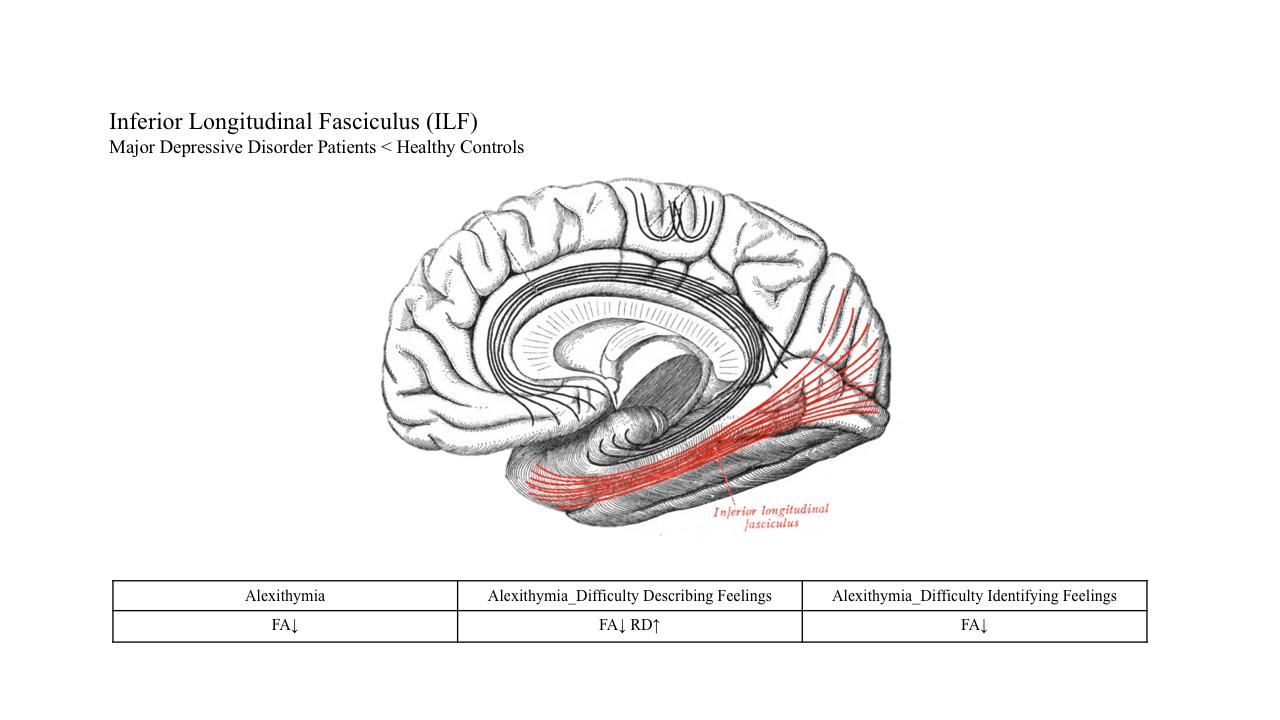
Patients with MDD exhibited a significantly lower FA values in the left inferior longitudinal fasciculus (ILF) (p=5.77×10-4) compared with healthy individuals (Table 2, Fig. 1).
Correlation between TAS and left inferior longitudinal fasciculus
Table 3 illustrates all significant associations between TAS and left ILF. The study uncovered a significant negative correlation between TAS score and FA of left ILF. The FA value of left ILF was negatively correlated with the total TAS score (r=-0.459, p=1.59×10-6), DDF (r=-0.346, p=4.14×10-4), and DIF (r=-0.408, p=2.51×10-5).
On the contrary, the AD, RD, MD values of left ILF exhibited positive correlations with the total TAS score. RD values of the left ILF, in particular, showed statistically significant associations with DDF (r=0.270, p=1.19×10-4).
The correlational study also exposed a strong correlation between depression severity and TAS and its subscales.
Correlation between TAS and symptoms of depression
In the secondary analysis of severity of depression, the subcategorized symptoms of depressed mood, feelings of guilt, suicidal ideation, and work and activities showed significant positive correlations with TAS within MDD group after the Bonferroni correction (Table 4). While the overall TAS score and DDF was significantly correlated with depressed mood (r=0.382, p=9.71×10-5; r=0.342, p=5.26×10-4), feelings of guilt (r=0.343, p=5.01×10-4; r=0.311, p=8.51×10-6), suicidal ideation (r=0.324, p=1.07×10-3; r=0.553, p=3.04×10-9), and work and activities (r=0.457, p=2.12×10-6; r=0.358, p=2.79×10-4), DIF only showed significant association with feelings of guilt (r=0.338, p=6.16×10-4).
In the further assessment of the influence of severity of depression, we have analyzed the difference in DTI scalar values with depression severity as an additional covariate. The analysis identified additional tracts with significant difference between MDD and HC (Table 5).
DISCUSSION
To the best of our knowledge, the present study is the first exhibiting a TRACULA approach to find potential association between WM tracts integrity and alexithymia in MDD. We have observed a significantly lower FA value in the left ILF in patients with MDD compared to HCs. We also discovered significant negative correlations between FA value of the left ILF with the total TAS score (r=-0.459, p=1.59×10-6), DDF (r=-0.346, p=4.14×10-4), and DIF (r=-0.408, p=2.51×10-5). Additionally, a significant positive correlation between RD value of the left ILF and DDF (r=0.270, p=1.19×10-4) was identified.
The reduced FA value of the left ILF in MDD is in line with previous studies [24, 29-32]. The ILF is a multidimensional, bidirectional association fiber tract that connects the occipital and temporal lobes, including the hippocampus and amygdala, which are the main components of the limbic system [33, 34]. The high association between limbic system dysfunction and increased risk for depression had been repeatedly explored and reported [35-38] and there is extensive evidence for increased activation in limbic areas in depression under exposure to emotional stimuli [39-42]. Furthermore, the alterations in the core regions of the limbic system in MDD is widely supported by structural studies reporting decreased volumes in the hippocampus [38, 43, 44] and anterior cingulate cortex [38]. The dysfunction within and between such structures may indicate a disturbance in emotional behavior and other cognitive aspects of depressive symptoms. Thus, the disconnection of the regions insinuated by the reduced FA values of the ILF, may be a predisposition for individuals to depressive symptoms. Moreover, from a functional perspective, the ILF is involved in processing and modulating visual cues and may constitute the pathophysiologic basis for socio-emotional impairments [33, 45].
As reported in previous studies [11-13, 21, 22], alexithymia has been associated with alterations in the CC, SLF, and ILF. In the present study, the left ILF was the tract that exhibited statistically significant group-wise difference. Consequently, we have selected it as a tract of interest and explored its potential associations with alexithymia. We observed negative correlations between FA value of the left ILF with the total TAS score, DDF, and DIF and positive correlation between RD value of the left ILF with DDF, which were in line with our initial hypothesis. As the FA index is a summary measure of WM integrity and AD, RD, and MD combine to produce significant alterations in the extent of directional diffusion relating to both myelination and axonal integrity, the associations altogether reflect the disturbance in the WM integrity with alexithymia [46, 47]. Various studies have made attempts to expose the underlying neuroanatomical bases of emotional experience and regulations, especially in the aspect of expressive suppression. Aforementioned Grabe et al. [20], have reported that changes in gray matter volume in regions including the dorsal anterior cingulate cortex, left insula, and inferior temporal gyrus were associated with difficulty identifying emotion and difficulty describing emotion. In parallel with our findings, no significant associations were found with externally-oriented thinking. The regions implicated in cognitive and attentional processes were also reported in individuals with deficiencies identifying, analyzing, and verbalizing feelings in other studies [48, 49]. Many have also insisted a key role of amygdala in alexithymia neuroimaging as the node of emotional perception system [50, 51]. The ILF, as a part of the major occipito-temporal associative tract [52], is a direct pathway between lingual cortex and amygdala. It is known to be involved in the limbic modulation of visual processing [53]. Given the cross-sectional nature of our study, it is impossible to evaluate the causal relationships between low FA value of ILF and alexithymia. However, our results may imply that impaired emotional self-awareness shares a neural foundation for the impaired cognitive domains including language processing, social cognition, and socio-emotional processing. We, thus, can derive the potential role of ILF in alexithymia as the main tract that connects multiple regions previously reported to have significant associations with alexithymia. The results comprehensively confirm that the integrity of ILF may be compromised in individuals having a hard time defining and identifying emotions.
Consistent with previous studies [3, 4, 8], the group comparison of TAS disclosed an association between MDD and alexithymia. The significantly higher scores for the total and the subscales of TAS in patients with MDD imply that the patients have large difficulties in various aspects of emotional processing. Moreover, the strong correlation between HDRS and TAS also indicate the potential relationship between illness severity and self-emotional processing. Our result confirms previous findings of the significant relationship between alexithymia and the severity of depression [54-57]. After controlling for depression severity, additional tracts have bared significant difference between MDD and HC (Table 5). As the direct causal relationship between depression severity and TAS has not yet been defined, we did not include it as a nuisance factor in our primary analysis. Nonetheless, we cannot exclude severity of depression as a confounding factor and acknowledge the potential influence of severity of depression in white matter tracts. A secondary analysis was then performed to further explore the strong correlation between TAS and depression symptom severity and exposed significant positive correlations in TAS with the subcategorized symptoms of depressed mood, feelings of guilt, suicidal ideation, and work and activities. Although, not a lot of studies examined the roles of symptoms of depression and alexithymia, a study assessed the interceding roles of shame and guilt in the associations between alexithymia, psychological distress, and suicide-related behaviors [58]. The study identified guilt as a mediation factor between both identification of feelings, description of feelings, and suicide-related behaviors. A systematic review also revealed strong relationships between alexithymia and the subcomponents of difficulty identifying and describing feelings but not externally-oriented thinking [59]. Our results, therefore, may indicate that people who have difficulty regulating their emotions collectively have greater risk of feeling guilt, decreased productivity, and engaging in self-injury [60, 61].
Despite such strengths, this study has several limitations. This is a cross-sectional study, which cannot inspect the causal relationships. We strongly insist on future longitudinal studies to gain a fuller understanding of the WM changes and alexithymia in MDD. Furthermore, patients under medications were included in the study, and thus, we are not free from the potential influence of medications in WM changes and alexithymic traits. We also only introduce WM tracts with significant associations with TAS and exhibiting group-wise differences potentially confounding how the neural changes lead to or from alexithymia and if the altered tracts predispose an individual to alexithymia. Lastly, although not small, a larger sample size in the future would be beneficial in validating and generalizing the results of this study.
In conclusion, the current study provided a basis for the brain changes regarding alexithymia in MDD patients. Left ILF had significant FA value change in patients with MDD and it was also negatively associated with alexithymia. The results suggest that these WM regions may be an important underlying pathology of compromised emotional self-recognition in MDD. Moreover, as the regions that ILF connects share a neural bases with impaired cognitive domains, especially in language processing, visual processing, and social cognition, we hope that our findings may provide a deeper understanding of the neural correlations behind the emotional processing in MDD.
ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF2020M3E5D9080792).
Figures
Tables
Demographic and clinical characteristics of patients with major depressive disorder and healthy controls.
| Characteristics | MDD (n=101) | HC (n=99) | p-value (t, c2) |
|---|---|---|---|
| Age | 33.47±12.45 | 35.91±13.26 | 0.181 (t=-1.344) |
| Sex (female/male) | 54/47 | 63/36 | 0.146 (chi2=2.130) |
| Education level | |||
| <10 years | 5 | 1 | |
| 10~16 years | 91 | 92 | 0.221 (chi2=2.743) |
| >16 years | 5 | 6 | |
| HDRS-17 score | 16.51±5.79 | 0.60±1.33 | <0.001 (t=26.676) |
| TICV (cm3) | 1,461.43±170.60 | 1,466.94±148.85 | 0.808 (t=-0.243) |
| TAS | 63.23±9.19 | 39.37±5.79 | <0.001 (t=19.852) |
| TAS_Difficulty describing feelings | 17.94±3.63 | 10.06±3.21 | <0.001 (t=16.252) |
| TAS_Difficulty identifying feelings | 22.91±5.63 | 10.71±3.52 | <0.001 (t=18.349) |
| TAS_Externaly-oriented thinking | 22.38±3.76 | 18.61±3.66 | <0.001 (t=7.185) |
| Medication, n | |||
| Antidepressants | |||
| SSRI | 13 | NA | |
| SNRI | 3 | ||
| NDRI | 1 | ||
| NaSSA | 1 | ||
| Etc | 3 | ||
| Combination of AD | 34 | ||
| Antipsychotics | |||
| AP | 16 | ||
| Combination of AP | 2 |
Data are mean±standard deviation for age, HDRS-17 scores, illness duration, and TICV. p-values for distribution of sex and education level were obtained using a chi-squared test. P-values for comparisons of age, HDRS scores, and TICV were obtained using an independent t-test.
HCs, healthy controls; MDD, Major depressive disorder; HDRS-17, 17-item Hamilton Depression Rating Scale; TICV, total intracranial cavity volume; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor; NDRI, norepinephrine-dopamine reuptake inhibitor; NaSSA, noradrenergic and specific serotonergic antidepressant; Combination of AD, combinations of two or more types of antidepressant; APs, antipsychotics; ADs, antidepressants.
Significant change in white matter tracts between MDD patients and HC
| Tract of interest | MDD (n=101) | HC (n=99) | MDD vs. HC | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F | p-value | |
| FA | ||||||
| Left ILF | 0.48 | 0.02 | 0.49 | 0.03 | 12.247 | 0.001 |
The F and p values were obtained using one-way analysis of covariance (ANCOVA) with the adjustment for age, sex, and education level as covariates.
MDD, patients with major depressive disorder; HC, healthy control participants; SD, standard deviation; ILF, inferior longitudinal fasciculus.
Bonferroni correction was applied: p<0.05/72=0.00069.
Partial correlations between scores on Toronto Alexithymia Scale subscales, HDRS, and white matter tracts in MDD
| TAS | TAS_DDF | TAS_DIF | TAS_EOT | HDRS | |
|---|---|---|---|---|---|
| TAS | - | ||||
| TAS_DDS | 0.952 | ||||
| TAS_DIF | 0.903 | 0.743 | |||
| TAS_EOT | 0.633 | 0.432 | 0.451 | ||
| HDRS | 0.756 | 0.720 | 0.731 | 0.419 | |
| FA | |||||
| Left ILF | -0.459 | -0.346 | -0.408 | -0.184 | -0.084 |
| AD | |||||
| Left ILF | 0.142 | 0.040 | 0.118 | 0.131 | -0.355 |
| RD | |||||
| Left ILF | 0.156 | 0.270 | 0.121 | 0.087 | 0.074 |
| MD | |||||
| Left ILF | 0.178 | 0.089 | 0.125 | 0.112 | -0.319 |
TAS, Toronto Alexithymia Scale; DDF, difficulty describing feelings; DIF, difficulty identifying feelings; EOT, externally-oriented thinking; HDRS, Hamilton Depression Rating Scale; ILF, inferior longitudinal fasciculus.
Bonferroni correction was applied: p<0.05/20=0.0025.
Significant correlations were presented in a bold face.
Correlational analysis between scores on Toronto Alexithymia Scale subscales and the subcategorized symptoms of depression
| TAS | TAS_DDF | TAS_DIF | TAS_EOT | |
|---|---|---|---|---|
| Depressed mood | 0.382 | 0.342 | 0.074 | 0.116 |
| Feelings of guilt | 0.343 | 0.311 | 0.338 | 0.101 |
| Suicidal ideation | 0.324 | 0.553 | 0.144 | 0.134 |
| Work and activities | 0.457 | 0.358 | 0.147 | 0.015 |
TAS, Toronto Alexithymia Scale; DDF, difficulty describing feelings; DIF, difficulty identifying feelings; EOT, externally-oriented thinking.
Bonferroni correction was applied: p<0.05/68=0.00074.
Significant correlations were presented in a bold face.
Significant change in white matter tracts between MDD patients and HC also controlling for depression severity
| Tract of interest | MDD (n = 101) | HC (n = 99) | MDD vs. HC | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | F | p-value | |||
| AD | ||||||||
| Left SLFP | 1.14×10-3 | 6.71×10-5 | 1.12×10-3 | 5.48×10-5 | 15.574 | 1.11×10-4 | ||
| Left SLFT | 1.18×10-3 | 6.07×10-5 | 1.17×10-3 | 5.09×10-5 | 15.155 | 1.36×10-4 | ||
| Left UNC | 1.20×10-3 | 5.70×10-5 | 1.12×10-3 | 5.44×10-5 | 12.127 | 6.14×10-4 | ||
| Right SLFP | 1.11×10-3 | 7.11×10-5 | 1.10×10-3 | 6.59×10-5 | 12.536 | 5.00×10-4 | ||
| RD | ||||||||
| Left CST | 4.91×10-4 | 4.69×10-5 | 4.83×10-4 | 4.30×10-5 | 15.258 | 1.29×10-4 | ||
| Left ILF | 5.77×10-4 | 4.06×10-5 | 5.64×10-4 | 3.56×10-5 | 13.971 | 2.44×10-4 | ||
| Left SLFP | 5.75×10-4 | 4.12×10-5 | 5.67×10-4 | 3.73×10-5 | 14.059 | 2.34×10-4 | ||
| Left SLFT | 5.60×10-4 | 4.02×10-5 | 5.50×10-4 | 3.63×10-5 | 16.130 | 8.45×10-5 | ||
| Left UNC | 5.99×10-4 | 4.72×10-5 | 5.91×10-4 | 3.75×10-5 | 12.661 | 4.69×10-4 | ||
| Right CAB | 5.91×10-4 | 8.10×10-5 | 5.74×10-4 | 7.82×10-5 | 12.458 | 5.20×10-4 | ||
| Right SLFP | 5.49×10-4 | 5.12×10-5 | 5.38×10-4 | 4.68×10-5 | 13.126 | 3.72×10-4 | ||
| Right SLFT | 5.43×10-4 | 4.50×10-5 | 5.34×10-4 | 4.01×10-5 | 12.310 | 5.60×10-4 | ||
| MD | ||||||||
| Left CST | 7.34×10-4 | 5.08×10-5 | 7.30×10-4 | 4.42×10-5 | 15.815 | 9.85×10-5 | ||
| Left ILF | 8.04×10-4 | 4.56×10-5 | 7.95×10-4 | 3.97×10-5 | 12.588 | 4.87×10-4 | ||
| Left SLFP | 7.62×10-4 | 4.69×10-5 | 7.51×10-4 | 3.99×10-5 | 16.613 | 6.68×10-5 | ||
| Left SLFT | 7.65×10-4 | 4.51×10-5 | 7.56×10-4 | 3.75×10-5 | 17.775 | 3.81×10-5 | ||
| Left UNC | 7.99×10-4 | 4.63×10-5 | 7.88×10-4 | 3.76×10-5 | 15.503 | 1.15×10-4 | ||
| Right ATR | 7.44×10-4 | 4.29×10-5 | 7.35×10-4 | 3.87×10-5 | 12.526 | 5.02×10-4 | ||
| Right SLFP | 7.37×10-4 | 5.53×10-5 | 7.24×10-4 | 5.08×10-5 | 14.032 | 2.37×10-4 | ||
| Right SLFT | 7.42×10-4 | 5.30×10-5 | 7.33×10-4 | 4.75×10-5 | 11.967 | 6.66×10-4 | ||
The F and p values were obtained using one-way analysis of covariance (ANCOVA) with the adjustment for age, sex, depression severity and education level as covariates.
MDD, patients with major depressive disorder; HC, healthy control participants; SD, standard deviation; ATR, anterior thalamic radiations; CAB, cingulum - angular bundle; CST, corticospinal tract; ILF, inferior longitudinal fasciculus; SLFP, superior longitudinal fasciculus - parietal endings; SLFT, superior longitudinal fasciculus - temporal endings; UNC, uncinate fasciculus
Bonferroni correction was applied: p<0.05/72=0.00069
References
- National Institute of Mental Health (2022) Major depression [Internet]. National Institutes of Health, Bethesda (MD).
Available from: https://www.nimh.nih.gov/health/statistics/major-depression - Sifneos PE (1973) The prevalence of 'alexithymic' characteristics in psychosomatic patients. Psychother Psychosom 22:255-262
- Celikel FC, Kose S, Erkorkmaz U, Sayar K, Cumurcu BE, Cloninger CR (2010) Alexithymia and temperament and character model of personality in patients with major depressive disorder. Compr Psychiatry 51:64-70
- Ho NS, Wong MM, Lee TM (2016) Neural connectivity of alexithymia: Specific association with major depressive disorder. J Affect Disord 93:362-372
- Li S, Zhang B, Guo Y, Zhang J (2015) The association between alexithymia as assessed by the 20-item Toronto alexithymia scale and depression: a meta-analysis. Psychiatry Res 227:1-9
- Taylor GJ, Bagby RM, Parker JD (2003) The 20-item Toronto alexithymia scale. IV. Reliability and factorial validity in different languages and cultures. J Psychosom Res 55:277-283
- Honkalampi K, Saarinen P, Hintikka J, Virtanen V, Viinamäki H (1999) Factors associated with alexithymia in patients suffering from depression. Psychother Psychosom 68:270-275
- Honkalampi K, Koivumaa-Honkanen H, Lehto SM, Hintikka J, Haatainen K, Rissanen T, Viinamäki H (2010) Is alexithymia a risk factor for major depression, personality disorder, or alcohol use disorders? A prospective population-based study. J Psychosom Res 68:269-273
- Saarijärvi S, Salminen JK, Tamminen T, Aärelä E (1993) Alexithymia in psychiatric consultation-liaison patients. Gen Hosp Psychiatry 15:330-333
- Bermond B, Bierman DJ, Cladder MA, Moormann PP, Vorst HC (2010) The cognitive and affective alexithymia dimensions in the regulation of sympathetic responses. Int J Psychophysiol 75:227-233
- Hoppe KD, Bogen JE (1977) Alexithymia in twelve commissurotomized patients. Psychother Psychosom 28:148-155
- Larsen JK, Brand N, Bermond B, Hijman R (2003) Cognitive and emotional characteristics of alexithymia: a review of neurobiological studies. J Psychosom Res 54:533-541
- Romei V, De Gennaro L, Fratello F, Curcio G, Ferrara M, Pascual-Leone A, Bertini M (2008) Interhemispheric transfer deficit in alexithymia: a transcranial magnetic stimulation study. Psychother Psychosom 77:175-181
- Kano M, Endo Y, Fukudo S (2018) Association between alexithymia and functional gastrointestinal disorders. Front Psychol 9:599
- De Gucht V, Heiser W (2003) Alexithymia and somatisation: quantitative review of the literature. J Psychosom Res 54:425-434
- Nakao M, Barsky AJ (2007) Clinical application of somatosensory amplification in psychosomatic medicine. Biopsychosoc Med 1:17
- Wingbermühle E, Theunissen H, Verhoeven WM, Kessels RP, Egger JI (2012) The neurocognition of alexithymia: evidence from neuropsychological and neuroimaging studies. Acta Neuropsychiatr 24:67-80
- Chester DS, Pond RS Jr, DeWall CN (2015) Alexithymia is associated with blunted anterior cingulate response to social rejection: implications for daily rejection. Soc Cogn Affect Neurosci 10:517-522
- Lane RD, Reiman EM, Axelrod B, Yun LS, Holmes A, Schwartz GE (1998) Neural correlates of levels of emotional awareness. Evidence of an interaction between emotion and attention in the anterior cingulate cortex. J Cogn Neurosci 10:525-535
- Grabe HJ, Wittfeld K, Hegenscheid K, Hosten N, Lotze M, Janowitz D, Völzke H, John U, Barnow S, Freyberger HJ (2014) Alexithymia and brain gray matter volumes in a general population sample. Hum Brain Mapp 35:5932-5945
- Seyedmirzaei H, Shafie M, Kargar A, Golbahari A, Bijarchian M, Ahmadi S, Shahmohammadi A, Sadeghi M, Aarabi MH, Mayeli M (2022) White matter tracts associated with alexithymia and emotion regulation: a diffusion MRI study. J Affect Disord 314:271-280
- Kubota M, Miyata J, Sasamoto A, Kawada R, Fujimoto S, Tanaka Y, Sawamoto N, Fukuyama H, Takahashi H, Murai T (2012) Alexithymia and reduced white matter integrity in schizophrenia: a diffusion tensor imaging study on impaired emotional self-awareness. Schizophr Res 141:137-143
- Han KM, Won E, Kang J, Choi S, Kim A, Lee MS, Tae WS, Ham BJ (2017) TESC gene-regulating genetic variant (rs7294919) affects hippocampal subfield volumes and parahippocampal cingulum white matter integrity in major depressive disorder. J Psychiatr Res 93:20-29
- Won E, Kang J, Choi S, Kim A, Han KM, Yoon HK, Cho SH, Tae WS, Lee MS, Joe SH, Kim YK, Ham BJ (2017) The association between substance P and white matter integrity in medication-naive patients with major depressive disorder. Sci Rep 7:9707
- Yendiki A, Panneck P, Srinivasan P, Stevens A, Zöllei L, Augustinack J, Wang R, Salat D, Ehrlich S, Behrens T, Jbabdi S, Gollub R, Fischl B (2011) Automated probabilistic reconstruction of white-matter pathways in health and disease using an atlas of the underlying anatomy. Front Neuroinform 5:23
- Watanabe A, Nakamae T, Sakai Y, Nishida S, Abe Y, Yamada K, Yokota I, Narumoto J (2018) The detection of white matter alterations in obsessive-compulsive disorder revealed by TRActs constrained by underlying anatomy (TRACULA). Neuropsychiatr Dis Treat 14:1635-1643
- Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56-62
- Bagby RM, Parker JD, Taylor GJ (1994) The twenty-item Toronto alexithymia scale--I. Item selection and cross-validation of the factor structure. J Psychosom Res 38:23-32
- Hermesdorf M, Berger K, Szentkirályi A, Schwindt W, Dannlowski U, Wersching H (2017) Reduced fractional anisotropy in patients with major depressive disorder and associations with vascular stiffness. Neuroimage Clin 14:151-155
- Lim J, Sohn H, Kwon MS, Kim B (2021) White matter alterations associated with pro-inflammatory cytokines in patients with major depressive disorder. Clin Psychopharmacol Neurosci 19:449-458
- van Velzen LS, Kelly S, Isaev D, Aleman A, Aftanas LI, Bauer J, Baune BT, Brak IV, Carballedo A, Connolly CG, Couvy-Duchesne B, Cullen KR, Danilenko KV, Dannlowski U, Enneking V, Filimonova E, Förster K, Frodl T, Gotlib IH, Groenewold NA, Grotegerd D, Harris MA, Hatton SN, Hawkins EL, Hickie IB, Ho TC, Jansen A, Kircher T, Klimes-Dougan B, Kochunov P, Krug A, Lagopoulos J, Lee R, Lett TA, Li M, MacMaster FP, Martin NG, McIntosh AM, McLellan Q, Meinert S, Nenadić I, Osipov E, Penninx BWJH, Portella MJ, Repple J, Roos A, Sacchet MD, Sämann PG, Schnell K, Shen X, Sim K, Stein DJ, van Tol MJ, Tomyshev AS, Tozzi L, Veer IM, Vermeiren R, Vives-Gilabert Y, Walter H, Walter M, van der Wee NJA, van der Werff SJA, Schreiner MW, Whalley HC, Wright MJ, Yang TT, Zhu A, Veltman DJ, Thompson PM, Jahanshad N, Schmaal L (2020) White matter disturbances in major depressive disorder: a coordinated analysis across 20 international cohorts in the ENIGMA MDD working group. Mol Psychiatry 25:1511-1525
- Wu F, Tu Z, Sun J, Geng H, Zhou Y, Jiang X, Li H, Kong L (2020) Abnormal functional and structural connectivity of amygdala-prefrontal circuit in first-episode adolescent depression: a combined fMRI and DTI study. Front Psychiatry 10:983
- Ashtari M (2012) Anatomy and functional role of the inferior longitudinal fasciculus: a search that has just begun. Dev Med Child Neurol 54:6-7
- Catani M, Jones DK, Donato R, Ffytche DH (2003) Occipito-temporal connections in the human brain. Brain 126(Pt 9):2093-2107
- Fournier JC, Keener MT, Almeida J, Kronhaus DM, Phillips ML (2013) Amygdala and whole-brain activity to emotional faces distinguishes major depressive disorder and bipolar disorder. Bipolar Disord 15:741-752
- Grotegerd D, Stuhrmann A, Kugel H, Schmidt S, Redlich R, Zwanzger P, Rauch AV, Heindel W, Zwitserlood P, Arolt V, Suslow T, Dannlowski U (2014) Amygdala excitability to subliminally presented emotional faces distinguishes unipolar and bipolar depression: an fMRI and pattern classification study. Hum Brain Mapp 35:2995-3007
- Becker G, Berg D, Lesch KP, Becker T (2001) Basal limbic system alteration in major depression: a hypothesis supported by transcranial sonography and MRI findings. Int J Neuropsychopharmacol 4:21-31
- Chen L, Wang Y, Niu C, Zhong S, Hu H, Chen P, Zhang S, Chen G, Deng F, Lai S, Wang J, Huang L, Huang R (2018) Common and distinct abnormal frontal-limbic system structural and functional patterns in patients with major depression and bipolar disorder. Neuroimage Clin 20:42-50
- Roffman JL, Marci CD, Glick DM, Dougherty DD, Rauch SL (2005) Neuroimaging and the functional neuroanatomy of psychotherapy. Psychol Med 35:1385-1398
- Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA (2001) Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry 50:651-658
- Fu CH, Williams SC, Cleare AJ, Brammer MJ, Walsh ND, Kim J, Andrew CM, Pich EM, Williams PM, Reed LJ, Mitterschiffthaler MT, Suckling J, Bullmore ET (2004) Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry 61:877-889
- Buchheim A, Viviani R, Kessler H, Kächele H, Cierpka M, Roth G, George C, Kernberg OF, Bruns G, Taubner S (2012) Changes in prefrontal-limbic function in major depression after 15 months of long-term psychotherapy. PLoS One 7:e33745
- Frodl T, O'Keane V (2013) How does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humans. Neurobiol Dis 52:24-37
- Musazzi L, Racagni G, Popoli M (2011) Stress, glucocorticoids and glutamate release: effects of antidepressant drugs. Neurochem Int 59:138-149
- Herbet G, Zemmoura I, Duffau H (2018) Functional anatomy of the inferior longitudinal fasciculus: from historical reports to current hypotheses. Front Neuroanat 12:77
- Coloigner J, Batail JM, Commowick O, Corouge I, Robert G, Barillot C, Drapier D (2019) White matter abnormalities in depression: a categorical and phenotypic diffusion MRI study. Neuroimage Clin 22:101710
- Hayakawa YK, Sasaki H, Takao H, Hayashi N, Kunimatsu A, Ohtomo K, Aoki S (2014) Depressive symptoms and neuroanatomical structures in community-dwelling women: a combined voxel-based morphometry and diffusion tensor imaging study with tract-based spatial statistics. Neuroimage Clin 4:481-487
- Goerlich-Dobre KS, Votinov M, Habel U, Pripfl J, Lamm C (2015) Neuroanatomical profiles of alexithymia dimensions and subtypes. Hum Brain Mapp 36:3805-3818
- van der Velde J, van Tol MJ, Goerlich-Dobre KS, Gromann PM, Swart M, de Haan L, Wiersma D, Bruggeman R, Krabbendam L, Aleman A (2014) Dissociable morphometric profiles of the affective and cognitive dimensions of alexithymia. Cortex 54:190-199
- Goerlich KS (2018) The multifaceted nature of alexithymia - a neuroscientific perspective. Front Psychol 9:1614
- Farah T, Ling S, Raine A, Yang Y, Schug R (2018) Alexithymia and reactive aggression: the role of the amygdala. Psychiatry Res Neuroimaging 281:85-91
- Crosby EC (1963) Correlative anatomy of the nervous system. J Med Educ 38:526
- Latini F (2015) New insights in the limbic modulation of visual inputs: the role of the inferior longitudinal fasciculus and the Li-Am bundle. Neurosurg Rev 38:179-189
- Bamonti PM, Heisel MJ, Topciu RA, Franus N, Talbot NL, Duberstein PR (2010) Association of alexithymia and depression symptom severity in adults aged 50 years and older. Am J Geriatr Psychiatry 18:51-56
- Sagar R, Talwar S, Desai G, Chaturvedi SK (2021) Relationship between alexithymia and depression: a narrative review. Indian J Psychiatry 63:127-133
- Honkalampi K, Hintikka J, Laukkanen E, Lehtonen J, Viinamäki H (2001) Alexithymia and depression: a prospective study of patients with major depressive disorder. Psychosomatics 42:229-234
- Hemming L, Haddock G, Shaw J, Pratt D (2019) Alexithymia and its associations with depression, suicidality, and aggression: an overview of the literature. Front Psychiatry 10:203
- Rice SM, Kealy D, Oliffe JL, Treeby MS, Ogrodniczuk JS (2020) Shame and guilt mediate the effects of alexithymia on distress and suicide-related behaviours among men. Psychol Health Med 25:17-24
- Hemming L, Taylor P, Haddock G, Shaw J, Pratt D (2019) A systematic review and meta-analysis of the association between alexithymia and suicide ideation and behaviour. J Affect Disord 254:34-48
- Norman H, Borrill J (2015) The relationship between self-harm and alexithymia. Scand J Psychol 56:405-419
- Law KC, Khazem LR, Anestis MD (2015) The role of emotion dysregulation in suicide as considered through the ideation to action framework. Curr Opin Psychol 3:30-35





