Articles
Article Tools
Supplementary
Stats or Metrics
Article
Original Article
Exp Neurobiol 2023; 32(5): 313-327
Published online October 31, 2023
https://doi.org/10.5607/en23028
© The Korean Society for Brain and Neural Sciences
Lactobacillus reuteri ATG-F4 Alleviates Chronic Stress-induced Anhedonia by Modulating the Prefrontal Serotonergic System
Jiyun Lee1,2†, Eum-Ji Kim1†, Gun-Seok Park3†, Jeongseop Kim1,2, Tae-Eun Kim1,2, Yoo Jin Lee1, Juyi Park3, Jihee Kang3*, Ja Wook Koo1,2* and Tae-Yong Choi1*
1Emotion, Cognition, and Behavior Research Group, Korea Brain Research Institute (KBRI), Daegu 41062,
2Department of Brain Sciences, Daegu Gyeongbuk Institute of Science and Technology (DGIST), Daegu 42988,
3AtoGen Co., Ltd., Daejeon 34015, Korea
Correspondence to: *To whom correspondence should be addressed.
Jihee Kang, TEL: 82-42-931-8255, FAX: 82-42-931-8257
e-mail: jhkang@atogen.co.kr
Ja Wook Koo, TEL: 82-53-980-8430, FAX: 82-53-980-8399
e-mail: jawook.koo@kbri.re.kr
Tae-Yong Choi, TEL: 82-53-980-8439, FAX: 82-53-980-8399
e-mail: tychoi5667@kbri.re.kr
†These authors contributed equally to this article.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
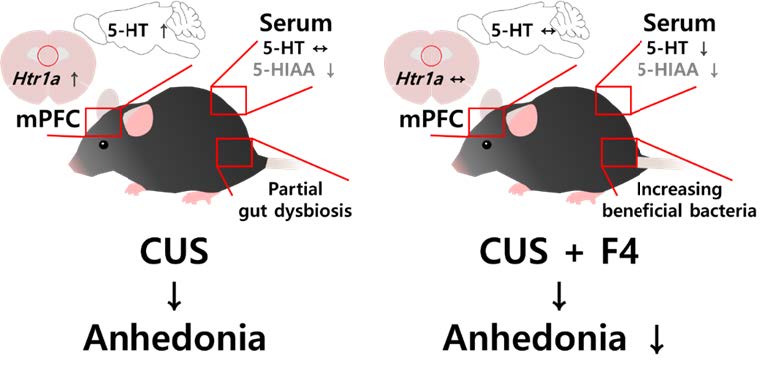
Mental health is influenced by the gut-brain axis; for example, gut dysbiosis has been observed in patients with major depressive disorder (MDD). Gut microbial changes by fecal microbiota transplantation or probiotics treatment reportedly modulates depressive symptoms. However, it remains unclear how gut dysbiosis contributes to mental dysfunction, and how correction of the gut microbiota alleviates neuropsychiatric disorders. Our previous study showed that chronic consumption of Lactobacillus reuteri ATG-F4 (F4) induced neurometabolic alterations in healthy mice. Here, we investigated whether F4 exerted therapeutic effects on depressive-like behavior by influencing the central nervous system. Using chronic unpredictable stress (CUS) to induce anhedonia, a key symptom of MDD, we found that chronic F4 consumption alleviated CUS-induced anhedonic behaviors, accompanied by biochemical changes in the gut, serum, and brain. Serum and brain metabolite concentrations involved in tryptophan metabolism were regulated by CUS and F4. F4 consumption reduced the elevated levels of serotonin (5-HT) in the brain observed in the CUS group. Additionally, the increased expression of Htr1a, a subtype of the 5-HT receptor, in the medial prefrontal cortex (mPFC) of stressed mice was restored to levels observed in stress-naïve mice following F4 supplementation. We further demonstrated the role of Htr1a using AAV-shRNA to downregulate Htr1a in the mPFC of CUS mice, effectively reversing CUS-induced anhedonic behavior. Together, our findings suggest F4 as a potential therapeutic approach for relieving some depressive symptoms and highlight the involvement of the tryptophan metabolism in mitigating CUS-induced depressive-like behaviors through the action of this bacterium.
Graphical Abstract
Keywords: Lactobacillus reuteri, Anhedonia, Prefrontal cortex, Serotonin
INTRODUCTION
Major depressive disorder (MDD), also known as depression, is a neuropsychiatric disease that negatively impacts an individual’s quality of life and burdens on society and the global economy [1-3]. It is characterized by various cognitive and psychophysical symptoms, including decreased motivation and persistent low mood [4]. Despite extensive research, the underlying mechanisms of MDD remains incompletely understood. However, accumulating evidence suggests that depression may be modulated by heterogeneous factors, from intrinsic to extrinsic [5]. Chronic stress originating from internal or external sources is a significant risk factor for depression. Prolonged exposure to stressors can disrupt the normal functioning of the neurotransmitter system, leading to psychophysical malfunction [6, 7]. Decades of animal studies have provided substantial evidence to support the chronic stress hypothesis, demonstrating similarities in symptomology between animal models and patients with depression [8, 9]. The chronic unpredictable stress (CUS) rodent model is widely recognized as a well-validated animal model for stress-induced depression. This model employs a variety of mild stressors to ensure high construct validity. Rodents who have experienced CUS consistently exhibit anhedonia, characterized by the inability to feel pleasure under normally pleasurable conditions, as a prominent feature alongside other depressive-like symptoms [10]. In addition, CUS-exposed mice often shown comprehensive physiological changes, including alterations in neurotransmitter systems [11-14].
Approximately one-third of patients with depression do not respond to conventional antidepressant drug therapies that primarily target the fine-tunning of neurotransmitters [15, 16]. As a result, there has been growing interest in novel therapeutic approaches, along with the pathophysiology of depression. Over the past decade, an increasing number of studies have investigated the relationship between depression and the gut-brain axis [17]. The gut-brain axis is a bidirectional signaling network that involves interactions among the intestinal microbiota, microbial metabolites, enteric nervous system, and neuroendocrine system [18]. Depending on the bacterial strain, the gut microbial environment generates neuroactive compounds, including neurotransmitters, amino acids, and microbial metabolites, that influence the nervous system. Bidirectional communication between bacterial strains and the central nervous system occurs through various biological pathways that modulate brain physiology. Alterations in the gut-brain axis can contribute to neuropsychiatric dysfunction. Conversely, restoring healthy gut microbial conditions may potentially improve mental disorders [19]. Probiotics are living microorganisms that have been suggested as a potential therapeutic strategy for treating depression by restoring the composition of gut microbiota [20, 21]. Preclinical studies have demonstrated the antidepressant-like effects of several probiotics in rodents, despite their underlying biological mechanisms [21]. In our previous study, we found that some
This study aimed to explore the potential of probiotic treatment in alleviating depressive-like behaviors, specifically anhedonia, induced by chronic stress. To investigate this, we administered F4 during CUS to examine its effects on CUS-induced anhedonic behaviors. We analyzed changes in the gut microbiota and metabolites to identify potential candidates involved in neurometabolic processes in the serum and brain. We identified changes in tryptophan metabolites in the serum and brain. Particularly, we observed increased 5-HT levels in the brains of chronically stressed mice, which were decreased by F4 treatment. Similarly, the enhancement of 5-HT1A receptor in the medial prefrontal cortex (mPFC) by CUS was restored by F4 supplementation. Finally, we confirmed that the prefrontal serotonergic system is associated with anhedonic behavior using adeno-associated virus (AAV)-mediated gene expression level adjustment. Overall, these findings suggest that the F4 strain alleviates chronic stress-induced anhedonic behaviors by modulating tryptophan metabolism and the prefrontal serotonergic system.
MATERIALS AND METHODS
Animals
Entire procedures using animals were approved by the Institutional Animal Care and Use Committee of Korea Brain Research Institute (IACUC-20-00023, IACUC-21-00006). 6-to-12-week-old C57BL6/N male mice (Orient-Bio Company, Busan, Republic of Korea) were employed in this study. Mice were maintained in a plastic cage under 24±2°C, 8:00~20:00 light/dark cycle in SPF grade animal facility. Also, mice were allowed to access chow and water ad libitum. Mice were group-housed during the chronic unpredictable stress (CUS) period. In the
Chronic unpredictable stress (CUS)
CUS was performed as previously described [23, 24]. In brief, eight-week-old mice received 28 days of CUS. Various stressors were intentionally designed to maximize unpredictable effects. All CUS mice were exposed to two or three stressors per day for 28 days. After the 28th day of the CUS, the mice’s body weight was measured. And three days of sucrose preference test were followed. In the CUS schedule, stressors are randomly arranged to prevent subjects from predicting. Well-validated stressors were applied from the following list: cage tilt 45º for overnight, food deprivation for overnight, water deprivation for overnight, strobe light for overnight, bedding removal for overnight, wet bedding for overnight, housed with different inmates for overnight, cage rotation for an hour, swimming stress for 5 minutes, light off during the daytime for 3 hours, restraint stress for an hour.
Sucrose preference test (SPT)
On the last day of the CUS period, mice were single-housed and the water bottles were removed until 4 p.m. After the water restriction, mice were provided with a 1% sucrose-water solution (w/v) and a water bottle. Following three consecutive days, SPT was performed two-bottled choice of water and 1% sucrose-water solution (w/v) from 4 p.m. to the next day at 10 a.m. for three sessions. Each bottle was weighed at 4 p.m. and 10 a.m. to calculate preference for each session. The positions of the bottles were counterbalanced every session to prevent a place preference. Sucrose preference was calculated as a percentage using this formula: average of {1% sucrose solution intake/total (1% sucrose solution+water) intake}*100 (%). And sucrose preference was shown as an average value of three sessions.
Lactobacillus strains
The anonymous donor of Daejeon, South Korea, kindly provided fecal samples of newborn babies and
For scrutinizing the anti-anhedonic effects of F4 on chronic unpredictable stress, mice were separated into three groups. During the CUS timespan, mice received phosphate-buffered saline (PBS) containing freeze-dried F4 powder
Sample extraction
One day after the last behavior test finished, the mice were anesthetized with the carbon dioxide (CO2) gas. Subsequently, the mice were laparotized and blood collection was performed using cardiac puncture. Cecal sample was collected by a cutoff using operation scissors. And the brain was removed from its head. All procedure was performed rapidly. Also, collected samples were placed immediately in -80°C deep freezer.
To perform real-time quantitative polymerase chain reaction (RT-qPCR) brain samples were sliced 1 mm coronal into the brain matrices. Target regions were micro-dissected from the applicable sections using tissue 14-gauge microdissection punches (BP-10F, Kai Medical). Regions of interest were the medial prefrontal cortex (mPFC), ventral hippocampus (vHIP), and basolateral amygdala (BLA).
Cecal microbiota analysis
Genomic DNA was extracted from fecal samples using the QIAamp PowerFecal Pro DNA Kit (QIAGEN). The quantity and quality of extracted DNA were measured using a Qubit 3.0 Fluorometer (Thermo Fisher Scientific) and agarose gel electrophoresis, respectively. The V4 hypervariable regions of the bacterial 16S rRNA were amplified with unique 8 bp barcodes and sequenced on the Illumina MiSeq PE300 platform according to the standard protocol [25]. Raw reads were analyzed using the QIIME pipeline [26] with the SILVA 132 database [27]. The non-parametric Kruskal-Wallis test was used to compare the differences in diversity indices and microbial taxa. The weighted UniFrac distances were previously obtained and used for PCoA [28].
LC-MS/MS instrumentation and analytical conditions
Tryptophan, kynurenine, kynurenic acid, tryptamine, 5-Hydroxytraptophan (5-HTP), serotonin (5-HT), and 5-Hydroxydindoleacetic acid (5-HIAA) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Ammonium formate (≥99.995% purity), formic acid (≥99.5% purity), high-performance liquid chromatography (HPLC) grade methanol (MeOH), HPLC grade acetonitrile (ACN) and HPLC grade water were purchased from Sigma-Aldrich. To prepare the samples, A 100 μl aliquot of serum was mixed with 500 μl of ice-cold MeOH with 1% formic acid. The brain tissue was homogenized in ice-cold MeOH with 1% formic acid (per gram of tissue by adding 4.0 ml of solution). The solution was mixed by vortex for 20 minutes and left for 2 h (4°C) to solidify the protein precipitate. After centrifugation at 14,000 rpm for 30 min at 4°C, the supernatant was filtrated by using a PVDF syringe filter (0.22 μm pore size) (Millipore, Billerica, MA). The filtered sample was then injected into the liquid chromatography-tandem mass spectrometry (LC-MS/MS) system. LC-MS/MS analyses were carried out using an Exion LC system connected to a QTRAP 4500 mass spectrometer (AB SCIEX, Framingham, MA, USA). For the analysis of Trp, 5-HT, MLT and 5-HIAA, the LC analyses were carried out using an Intrada Amino Acid column (150×2 mm, 3-μm particle size, Imtakt Kyoto, JPN). A 5 μl aliquot was used for the autosampler injection, and the flow rate was 0.6 ml/min at 40°C. A gradient mobile phase, consisting of (A) 100 mM Ammonium formate/ACN (80/20, v/v) solution and (B) 0.3% formic acid in ACN solution, was used. The gradient started at 80% B and was held at this value for 4 min. It then increased linearly to 0% B over 10 minutes, followed by a 2-minute hold at 0% B before returning to 80% B in 0.1 minute. Finally, the gradient was kept at 80% B for 8.9 min to re-equilibrate the column. The total analysis time was 25 min. For the analysis of KYN, KYNA, tryptamine and 5-HTP, the LC analyses were carried out using an ACQUITY UPLC HSS PFP VanGuard Pre-column (5×2.1 mm, 1.8-μm particle size, Waters, MA, USA) and ACQUITY UPLC HSS PFP Column, (100×2.1 mm, 1.8-μm particle size, Waters). A 2 μl aliquot was used for the autosampler injection, and the flow rate was 0.2 ml/min at 40°C. A gradient mobile phase was employed, consisting of (A) 0.2% formic acid in water solution and (B) 0.2% formic acid in MeOH/ACN (50/50, v/v) solution. The gradient started at 0% B and was held at this value for 0.5 min. The gradient increased linearly to 10% B in 2.5 min, 70% B in 1 min and 90% B in 4 min. Finally, the gradient was kept at 0% B for 7 min. The total analysis time was 15 min. The analysis was performed using an electrospray ionization source in positive mode. The operation conditions were as follows: ion spray voltage, 5500 V; curtain gas (CUR), 25 psi; collision gas (CAD), medium; ion source gas 1 (GS1) and ion source gas 2 (GS2), 50 and 50 psi; the turbo spray temperature (TEM), 450°C; entrance potential (EP), 10 V. Nitrogen was used in all cases. Analytes were quantificated by multiple reaction monitoring (MRM) employing the following precursor to product ion transitions and parameters: Trp, m/z 205.0→188.0 with declustering potential (DP) 61 V, collision energy (CE) 13 eV and collision cell exit potential (CXP), 10 V; KYN, m/z 209.0→94.0 with DP 6 V, CE 19 eV and CXP 8 V; KYNA, m/z 190.0→144.0 with DP 6 V, CE 27 eV and CXP 6 V; tryptamine, m/z 161.0→144.0 with DP 1 V, CE 19 eV and CXP 8 V; 5-HTP, m/z 221.1→204.1 with DP 61 V, CE 15 eV and CXP 8 V; 5-HT, m/z 177.1→160.0 with DP 46 V, CE 17 eV and CXP 8 V; MLT, m/z 233.1→174.1 with DP 61 V, CE 21 eV and CXP 12 V; 5-HIAA, m/z 192.0→146.1 with DP 1 V, CE 19 eV and CXP 10 V. SCIEX OS 2.0.0 software (AB SCIEX) was used for data acquisition and processing, and Analyst 3.3 software (AB SCIEX) was used for data analysis.
RNA extraction and RT-qPCR
The expression levels of
Total RNA from brain tissues was extracted using the RNeasy Mini Kit (QIAgen®, USA). Tissue homogenization was performed by adding QIAzol Lysis Buffer RLT (350 μl with 1% β-mercaptoethanol). Further extraction steps followed the manufacturer’s instructions, and each RNA sample was supplementarily treated with DNase I buffer (QIAgen®, USA).
All RNA samples were evaluated for concentration and purity using a 4200 TapeStation (Agilent Technologies, Santa Clara, USA). Each RNA sample has normalized the concentration across the samples, and cDNA was synthesized using iScript reverse-transcriptase (1708891, Bio-Rad, Hercules, USA).
Specific quantification of target cDNA was conducted using the LightCycler® 480 SYBR Green I Master (Roche, Basal, Switzerland) on Light Cycler 480II (Roche, Basal, Switzerland). Each cDNA sample was run in triplicate. Gene expression analysis was performed using the ΔΔCt method [29], with
Stereotaxic surgery
To identify
Histology
Mice were anesthetized with CO2 and transcardially perfused with 0.1 M phosphate-buffered saline (PBS) and 4% (w/v) paraformaldehyde (PFA) in PBS. Brains were removed, post-fixed overnight in 4% PFA, and then equilibrated in 30% sucrose in PBS at 4°C. 60 μm coronal sections containing mPFC were cut on a cryocut microtome (CM1860, Leica Biosystems) at -20°C. All sections were washed in PBS, mounted on a slide glass, and cover-slipped with VECTASIELD Hardset Antifade Mounting Medium with DAPI (H-1500, Vector Laboratories). Images were acquired using a fluorescence microscope (PANNORAMIC SCAN, 3DHISTEC Ltd.) with a 20× objective lens.
Statistical analysis
All statistical analyses were conducted using Prism 9 (GraphPad Software, USA). Normality (Shapiro-Wilk test) and equal variance (Bartlett’s test) were tested before parametric analysis. In experiment assessing
RESULTS
Anti-anhedonic effect of Lactobacillus reuteri ATG-F4
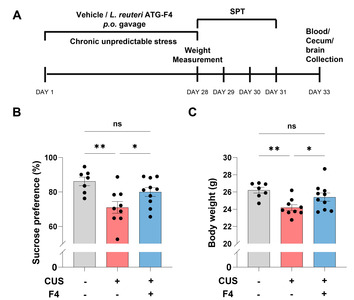
We conducted a sucrose preference test (SPT) to investigate whether F4 intake can alleviate anhedonia induced by CUS (Fig. 1A). Reduced interest in sweet solution indicates lower reward responsiveness, which is a decisive criterion for depression in human patients. Sucrose preference was significantly decreased in mice with CUS and vehicle (CUS+Veh) compared to control mice (Fig 1B). Mice treated with CUS and F4 (CUS+F4) showed rescue of sucrose preference compared to the CUS+Veh group (Fig. 1B). CUS also lowered the body weight, which was restored in the CUS+F4 group (Fig. 1C). These behavioral assays suggest that chronic F4 strain intake could recover CUS-induced anhedonia.
Modulation of caecal microbiota by F4
We analyzed the bacterial community from cecum samples to verify whether behavioral changes were related to the restoration of the gut microbiota by F4 intake. The 16S rRNA sequencing data showed that CUS partially, but not significantly, induced gut dysbiosis (Supplementary Fig. 1). Bacterial richness was measured using the Chao1, which indicates bacterial richness, and Shannon index, which indicates species diversity. Both indices showed that all groups were not significantly different (Supplementary Fig. 1A, B). Unweighted UniFrac-based principal coordinate analysis was performed to compare group differences in the overall microbiota profile (Supplementary Fig. 1C~E). In PCo2, the CUS+F4 group showed an approaching tendency to the control group compared with the CUS+Veh group (Supplementary Fig. 1E). At the genus level, populations of
Effects of CUS and F4 on 5-HT and tryptophan metabolic pathways in the serum and brain
Tryptophan is involved in separate metabolic pathways, including 5-HT synthesis and the kynurenine and indole pathways (Fig. 2A). Therefore, we checked whether CUS and F4 treatment changed tryptophan and its metabolites because 5-HT, a metabolite of tryptophan, is an important neurotransmitter related to depression [30]. First, we found that serum tryptophan was decreased by CUS, but this reduction was not reversed by F4 treatment (Fig. 2B). Although 5-hydroxytrptophan (5-HTP) levels showed a decreasing trend following CUS, it was not significant. However, they were significantly increased by F4 treatment (Fig. 2C). Despite decreased 5-HT levels in the CUS group, which tended to increase after F4 treatment, this change was not significant (Fig. 2D). This was similar to our previous findings, in which serum 5-HT levels decreased as a result of ampicillin-induced gut dysbiosis [22]. Based on these findings, we infer that F4 may improve the decrease in serum 5-HT levels caused by gut dysbiosis, although the exact mechanism is unknown. Similar to serum tryptophan, serum 5-hydroxyindoleacetic acid (5-HIAA), a 5-HT metabolite, and kynurenine, a major metabolite in the kynurenine pathway, were decreased by CUS and F4 treatment (Fig. 2E, F). Serum tryptamine, a major metabolite of the indole pathway, was reduced by CUS and this effect was rescued by F4 treatment (Fig. 2H). However, since changes in tryptophan metabolites in the serum cannot directly explain the antidepressant effects of F4, we examined the changes in tryptophan metabolites in the brain.
Brain tryptophan levels tended to decrease in response to CUS (Fig. 2I). We found that brain tryptophan levels were significantly decreased in the CUS+F4 group (Fig. 2I). These reductions were believed to be due to reduced tryptophan intake and serum tryptophan levels (Fig. 2B). Brain 5-HTP showed no differences among the three groups, but tended to be elevated in the CUS+Veh group (Fig. 2J). Next, brain 5-HT levels were increased by CUS and recovered by F4 treatment (Fig. 2K). While it remains unclear how F4 treatment during CUS lowered brain tryptophan levels, this is likely to be a major contributor to the reduction in brain 5-HT caused by F4. We considered that the increase in brain 5-HT was due to CUS and its decrease by F4 could be a key mechanism underlying the antidepressant effects of F4. CUS did not change the 5-HIAA levels in the brain, but it was significantly reduced in the CUS+F4 group (Fig. 2L). The similarity in the differences in brain 5-HT and 5-HIAA levels between the CUS+Veh and CUS+F4 groups suggests that the conversion of 5-HT to 5-HIAA by monoamine oxidase (MAO) may not be influenced by F4 treatment. Brain tryptamine levels were significantly altered; CUS-induced lower brain tryptamine levels, which were also significantly reduced in the F4 treatment group compared to those in the CUS+Veh group (Fig. 2O). This result implies that the indole pathway is prominently affected by CUS and F4 treatment. Contrastingly, brain kynurenine levels were similar among the control, CUS+Veh, and CUS+F4 groups (Fig. 2M). Additionally, kynurenic acid levels were significantly reduced in the CUS+F4 group (Fig. 2N). This indicates that CUS regulates the kynurenine pathway, and it is possible that F4 further modulated this pathway because there was a decrease in tryptophan in the CUS+F4 group without a corresponding change in kynurenine, but with kynurenic acid changes.
Effects of CUS and F4 on 5-HT receptor mRNA expression in the mPFC
To identify the biological correlates of behavioral and neurochemical changes in the brain, we measured the expression levels of the 5-HT receptors
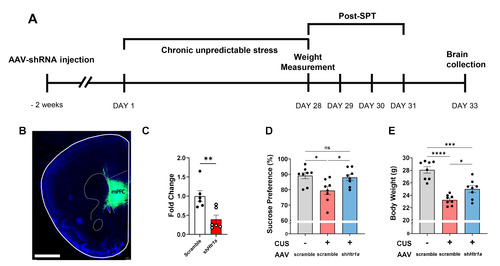
Recapitulation of the anti-anhedonic effect by Htr1a knockdown in the mPFC
We tested whether the balance of the serotonergic system in the mPFC mimicked the anti-anhedonic effects of the F4 treatment (Fig. 4A). The short hairpin RNA (shRNA) used to knockdown
DISCUSSION
This study investigated the effects of the F4 strain on CUS-induced anhedonia and explored its underlying mechanisms. Our results showed that F4 intake improved CUS-induced anhedonic behavior, as measured by the SPT (Fig. 1B). These improvements are likely attributable to the modulation of tryptophan metabolism and the serotonergic system in the mPFC (Fig. 3, 4).
Anhedonia, which is characterized by a diminished ability to experience pleasure, is a prominent behavioral feature of depression [10]. Lower reward responsiveness is a behavioral characteristic of CUS. Thus, the CUS mouse model is a valuable tool for investigating novel treatments for depression owing to its high validity. In the current study, F4 treatment of CUS-exposed animals resulted in the recovery of body weight reduction and elevated responsiveness to reward in the SPT (Fig. 1B, C). These results are consistent with the existing literature, suggesting that the administration of specific bacterial strains can alleviate depressive-like behaviors [31-33]. Thus, our results support the hypothesis that F4 exerts therapeutic effects on depressive symptoms.
In this study, 16S rRNA sequencing data showed no apparent alterations in the distribution of the gut microbial community (Supplementary Fig. 1). Overall, bacterial richness and diversity were not significantly affected by stress or F4 treatment (Supplementary Fig. 1A, B). Unlike previous studies [33, 34], our results indicate that neither stress nor F4 treatment combined with stress can modify gut microbial conditions. However, a few species of bacteria, such as
We quantified the primary metabolites in the 5-HT synthesis and tryptophan metabolism pathways in both the serum and brain to analyze how they were related to changes in anhedonia and body weight (Fig. 2). The relative abundance of metabolites between the groups varied in the serum and brain. Diverse biochemical compounds, including 5-HT, undergo independent metabolic pathways within the body that are distinct from those within the brain owing to the presence of the blood-brain barrier [36, 37]. However, changes in tryptophan-related metabolism have been observed in both the brain and serum under stressful conditions [38-40]. To begin with, examining the changes in 5-HT, the serum 5-HT level decreased due to CUS (Fig. 2D), which is consistent with the results of previous studies [33, 41-43]. The synthesis of 5-HT occurs in both the central nervous system and gastrointestinal tract [36, 44]. Regardless of the location in the gut-brain axis, the synthetic cascade is similar [36, 45]. 5-HT is synthesized from the amino acid tryptophan via a short metabolic pathway. Both 5-HTP and 5-HIAA are metabolites of the serotonin synthesis pathway [45]. Approximately 90% of 5-HT is produced in the gastrointestinal tract [36, 44], and 5-HT-related transmission is suggested to be one of the critical signaling pathways through the microbiota-gut-brain axis [46-48]. Several studies have suggested that the antidepressant-like effects of probiotics are associated with 5-HT synthesis and tryptophan metabolism [49-51]. Another animal model of depression utilizing chronic social defeat stress with different
Tryptophan is the primary component in 5-HT biosynthesis [45, 62]. However, the tryptophan metabolic pathway is not limited to 5-HT synthesis [45, 62, 63]. More than 90% of tryptophan is metabolized to kynurenine, which also participates in various metabolic pathways [45, 62]. Serum tryptophan levels significantly decreased under stress conditions (Fig. 2B). Lower plasma tryptophan levels have been observed in patients with MDD [64]. This suggests that the abundance of serum tryptophan may be a potential indicator of a stress condition. There were no significant differences in kynurenine levels in the brain (Fig. 2M). Contrastingly, serum kynurenine levels were lower in the CUS+Veh and CUS+F4 groups than those in the control group (Fig. 2F). Lower kynurenine levels were identified in a meta-analysis of MDD [65]. However, brain kynurenine levels were no significant differences among the groups. Unlike alterations in kynurenine levels, changes in kynurenic acid levels were observed only in the brain. Kynurenic acid levels were significantly lower in the CUS+F4 group than in the control group. The kynurenine pathway is also associated with inflammation. Kynurenic acid is an N-methyl-D-aspartate receptor (NMDAR) antagonist known for its protective effects against excitotoxic and apoptotic damage [63, 66]. However, in schizophrenia, elevated levels of kynurenine acid in the brain can lead to an excessive blockade of NMDAR, a known trigger of psychiatric symptoms [66]. A previous study reported that kynurenic acid in the postmortem PFC of the brain was increased in patients with schizophrenia patients who had higher levels of proinflammatory cytokines. This indicates that dysregulation of the kynurenine pathway can lead to neuropsychiatric diseases [67].
Tryptamine is a biochemical involved in the indole pathway. Tryptamine levels in the brain were significantly altered (Fig. 2O). In addition to the decrease in tryptamine levels in the CUS+Veh group compared to the control group, the CUS+F4 group exhibited a significant reduction in tryptamine levels compared to the CUS+Veh and control groups. Additionally, the serum tryptamine levels were altered (Fig. 2H). In the serum, the level of tryptamine was significantly lower in the CUS+Veh group than in the control group. Further, a significant increase in tryptamine levels was observed in the CUS+F4 group compared to that in the CUS+Veh group. Only a few studies have recognized tryptamine as a subtle neuromodulator of trace amine-associated receptor 1 (TAAR1) with the ability to influence neuronal cell responses independent of binding to postsynaptic receptors [68, 69]. Additionally, activation of TAAR1 suggests potential treatments for neuropsychiatric diseases [70, 71]. Thus, changes in tryptamine levels under stress conditions and F4 treatment are a possible candidates for the antidepressant-like effects of F4. While changes in brain 5-HT alterations are expected to play a significant role in behavioral changes during chronic stress, F4 influences various aspects of the tryptophan-involved metabolic pathways, including 5-HT synthesis, the kynurenine pathway, and the indole pathway. Since tryptophan metabolites are known to affect neuropsychiatric symptoms, further research is required to confirm the direct influence of F4.
We also analyzed the expression of 5-HT receptors in the mPFC, vHIP, and BLA, which are involved in depression and the serotonin pathway [53].
In summary, our findings demonstrate that the consumption of
Supplemental Materials
ACKNOWLEDGEMENTS
This research was supported by the KBRI Basic Research Program through Korea Brain Research Institute funded by Ministry of Science and ICT (23-BR-02-02 and 23-BR-02-07) and by AtoGen Co., Ltd..
Figures


References
- Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, Lund C, Medina Mora ME, Petersen I, Scott J, Shidhaye R, Vijayakumar L, Thornicroft G, Whiteford H; DCP MNS Author Group (2016) Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet 387:1672-1685
- Haroz EE, Ritchey M, Bass JK, Kohrt BA, Augustinavicius J, Michalopoulos L, Burkey MD, Bolton P (2017) How is depression experienced around the world? A systematic review of qualitative literature. Soc Sci Med 183:151-162
- Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, Haushofer J, Herrman H, Jordans M, Kieling C, Medina-Mora ME, Morgan E, Omigbodun O, Tol W, Patel V, Saxena S (2018) Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry 5:357-369
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. American Psychiatric Publishing, Arlington, VA
- Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF (2016) Major depressive disorder. Nat Rev Dis Primers 2:16065
- Tafet GE, Bernardini R (2003) Psychoneuroendocrinological links between chronic stress and depression. Prog Neuropsychopharmacol Biol Psychiatry 27:893-903
- Tafet GE, Nemeroff CB (2016) The links between stress and depression: psychoneuroendocrinological, genetic, and environmental interactions. J Neuropsychiatry Clin Neurosci 28:77-88
- Gururajan A, Reif A, Cryan JF, Slattery DA (2019) The future of rodent models in depression research. Nat Rev Neurosci 20:686-701
- Krishnan V, Nestler EJ (2011) Animal models of depression: molecular perspectives. Curr Top Behav Neurosci 7:121-147
- Willner P (1997) Validity, reliability and utility of the chronic mild stress model of depression: a 10-year review and evaluation. Psychopharmacology (Berl) 134:319-329
- Matuszewich L, McFadden LM, Friedman RD, Frye CA (2014) Neurochemical and behavioral effects of chronic unpredictable stress. Behav Pharmacol 25:557-566
- Sequeira-Cordero A, Salas-Bastos A, Fornaguera J, Brenes JC (2019) Behavioural characterisation of chronic unpredictable stress based on ethologically relevant paradigms in rats. Sci Rep 9:17403
- van Riel E, Meijer OC, Steenbergen PJ, Joëls M (2003) Chronic unpredictable stress causes attenuation of serotonin responses in cornu ammonis 1 pyramidal neurons. Neuroscience 120:649-658
- Lages YVM, Rossi AD, Krahe TE, Landeira-Fernandez J (2021) Effect of chronic unpredictable mild stress on the expression profile of serotonin receptors in rats and mice: a meta-analysis. Neurosci Biobehav Rev 124:78-88
- Al-Harbi KS (2012) Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence 6:369-388
- Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M (2006) Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 163:1905-1917
- Choi TY, Choi YP, Koo JW (2020) Mental disorders linked to crosstalk between the gut microbiome and the brain. Exp Neurobiol 29:403-416
- Foster JA, McVey Neufeld KA (2013) Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 36:305-312
- Cenit MC, Sanz Y, Codoñer-Franch P (2017) Influence of gut microbiota on neuropsychiatric disorders. World J Gastroenterol 23:5486-5498
- Liu RT, Walsh RFL, Sheehan AE (2019) Prebiotics and probiotics for depression and anxiety: a systematic review and meta-analysis of controlled clinical trials. Neurosci Biobehav Rev 102:13-23
- Yong SJ, Tong T, Chew J, Lim WL (2020) Antidepressive mechanisms of probiotics and their therapeutic potential. Front Neurosci 13:1361
- Beck BR, Park GS, Jeong DY, Lee YH, Im S, Song WH, Kang J (2019) Multidisciplinary and comparative investigations of potential psychobiotic effects of Lactobacillus strains isolated from newborns and their impact on gut microbiota and ileal transcriptome in a healthy murine model. Front Cell Infect Microbiol 9:269
- Koo JW, Duman RS (2008) IL-1beta is an essential mediator of the antineurogenic and anhedonic effects of stress. Proc Natl Acad Sci U S A 105:751-756
- Koo JW, Russo SJ, Ferguson D, Nestler EJ, Duman RS (2010) Nuclear factor-κB is a critical mediator of stress-impaired neurogenesis and depressive behavior. Proc Natl Acad Sci U S A 107:2669-2674
- Caporaso JG, Lauber CL, Walters WA, Berg-Lyons D, Huntley J, Fierer N, Owens SM, Betley J, Fraser L, Bauer M, Gormley N, Gilbert JA, Smith G, Knight R (2012) Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME J 6:1621-1624
- Caporaso JG, Kuczynski J, Stombaugh J, Bittinger K, Bushman FD, Costello EK, Fierer N, Peña AG, Goodrich JK, Gordon JI, Huttley GA, Kelley ST, Knights D, Koenig JE, Ley RE, Lozupone CA, McDonald D, Muegge BD, Pirrung M, Reeder J, Sevinsky JR, Turnbaugh PJ, Walters WA, Widmann J, Yatsunenko T, Zaneveld J, Knight R (2010) QIIME allows analysis of high-throughput community sequencing data. Nat Methods 7:335-336
- Yilmaz P, Parfrey LW, Yarza P, Gerken J, Pruesse E, Quast C, Schweer T, Peplies J, Ludwig W, Glöckner FO (2014) The SILVA and "All-Species Living Tree Project (LTP)" taxonomic frameworks. Nucleic Acids Res 42:D643-D648
- Lozupone C, Lladser ME, Knights D, Stombaugh J, Knight R (2011) UniFrac: an effective distance metric for microbial community comparison. ISME J 5:169-172
- Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25:402-408
- Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA (2022) The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. doi: 10.1038/s41380-022-01661-0
- Bharwani A, Mian MF, Surette MG, Bienenstock J, Forsythe P (2017) Oral treatment with Lactobacillus rhamnosus attenuates behavioural deficits and immune changes in chronic social stress. BMC Med 15:7
- Bercik P, Park AJ, Sinclair D, Khoshdel A, Lu J, Huang X, Deng Y, Blennerhassett PA, Fahnestock M, Moine D, Berger B, Huizinga JD, Kunze W, McLean PG, Bergonzelli GE, Collins SM, Verdu EF (2011) The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol Motil 23:1132-1139
- Xie R, Jiang P, Lin L, Jiang J, Yu B, Rao J, Liu H, Wei W, Qiao Y (2020) Oral treatment with Lactobacillus reuteri attenuates depressive-like behaviors and serotonin metabolism alterations induced by chronic social defeat stress. J Psychiatr Res 122:70-78
- Huang L, Lv X, Ze X, Ma Z, Zhang X, He R, Fan J, Zhang M, Sun B, Wang F, Liu H (2022) Combined probiotics attenuate chronic unpredictable mild stress-induced depressive-like and anxiety-like behaviors in rats. Front Psychiatry 13:990465
- Jiang H, Ling Z, Zhang Y, Mao H, Ma Z, Yin Y, Wang W, Tang W, Tan Z, Shi J, Li L, Ruan B (2015) Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav Immun 48:186-194
- El-Merahbi R, Löffler M, Mayer A, Sumara G (2015) The roles of peripheral serotonin in metabolic homeostasis. FEBS Lett 589:1728-1734
- Nakatani Y, Sato-Suzuki I, Tsujino N, Nakasato A, Seki Y, Fumoto M, Arita H (2008) Augmented brain 5-HT crosses the blood-brain barrier through the 5-HT transporter in rat. Eur J Neurosci 27:2466-2472
- Correia AS, Vale N (2022) Tryptophan metabolism in depression: a narrative review with a focus on serotonin and kynurenine pathways. Int J Mol Sci 23:8493
- Miura H, Ozaki N, Sawada M, Isobe K, Ohta T, Nagatsu T (2008) A link between stress and depression: shifts in the balance between the kynurenine and serotonin pathways of tryptophan metabolism and the etiology and pathophysiology of depression. Stress 11:198-209
- Karu N, McKercher C, Nichols DS, Davies N, Shellie RA, Hilder EF, Jose MD (2016) Tryptophan metabolism, its relation to inflammation and stress markers and association with psychological and cognitive functioning: Tasmanian Chronic Kidney Disease pilot study. BMC Nephrol 17:171
- Zhou Y, Cong Y, Liu H (2020) Folic acid ameliorates depression-like behaviour in a rat model of chronic unpredictable mild stress. BMC Neurosci 21:1
- Zhao J, Niu C, Wang J, Yang H, Du Y, Wei L, Li C (2018) The depressive-like behaviors of chronic unpredictable mild stress-treated mice, ameliorated by Tibetan medicine Zuotai: involvement in the hypothalamic-pituitary-adrenal (HPA) axis pathway. Neuropsychiatr Dis Treat 14:129-141
- Huang X, Li W, You B, Tang W, Gan T, Feng C, Li C, Yang R (2020) Serum metabonomic study on the antidepressant-like effects of ellagic acid in a chronic unpredictable mild stress-induced mouse model. J Agric Food Chem 68:9546-9556
- Berger M, Gray JA, Roth BL (2009) The expanded biology of serotonin. Annu Rev Med 60:355-366
- Höglund E, Øverli Ø, Winberg S (2019) Tryptophan metabolic pathways and brain serotonergic activity: a comparative review. Front Endocrinol (Lausanne) 10:158
- Layunta E, Buey B, Mesonero JE, Latorre E (2021) Crosstalk between intestinal serotonergic system and pattern recognition receptors on the microbiota-gut-brain axis. Front Endocrinol (Lausanne) 12:748254
- Carabotti M, Scirocco A, Maselli MA, Severi C (2015) The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol 28:203-209
- Yano JM, Yu K, Donaldson GP, Shastri GG, Ann P, Ma L, Nagler CR, Ismagilov RF, Mazmanian SK, Hsiao EY (2015) Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 161:264-276
- Wei CL, Wang S, Yen JT, Cheng YF, Liao CL, Hsu CC, Wu CC, Tsai YC (2019) Antidepressant-like activities of live and heat-killed Lactobacillus paracasei PS23 in chronic corticosterone-treated mice and possible mechanisms. Brain Res 1711:202-213
- Tian P, Wang G, Zhao J, Zhang H, Chen W (2019) Bifidobacterium with the role of 5-hydroxytryptophan synthesis regulation alleviates the symptom of depression and related microbiota dysbiosis. J Nutr Biochem 66:43-51
- Liang S, Wang T, Hu X, Luo J, Li W, Wu X, Duan Y, Jin F (2015) Administration of Lactobacillus helveticus NS8 improves behavioral, cognitive, and biochemical aberrations caused by chronic restraint stress. Neuroscience 310:561-577
- Ślifirski G, Król M, Turło J (2021) 5-HT receptors and the development of new antidepressants. Int J Mol Sci 22:9015
- Andrews PW, Bharwani A, Lee KR, Fox M, Thomson JA Jr (2015) Is serotonin an upper or a downer? The evolution of the serotonergic system and its role in depression and the antidepressant response. Neurosci Biobehav Rev 51:164-188
- Yohn CN, Gergues MM, Samuels BA (2017) The role of 5-HT receptors in depression. Mol Brain 10:28
- Kennett GA, Chaouloff F, Marcou M, Curzon G (1986) Female rats are more vulnerable than males in an animal model of depression: the possible role of serotonin. Brain Res 382:416-421
- Adell A, Garcia-Marquez C, Armario A, Gelpi E (1988) Chronic stress increases serotonin and noradrenaline in rat brain and sensitizes their responses to a further acute stress. J Neurochem 50:1678-1681
- Zhao H, Mohamed NE, Chan SJ, Tan CT, Tao R, Yu VC, Wong PT (2019) Absence of stress response in dorsal raphe nucleus in modulator of apoptosis 1-deficient mice. Mol Neurobiol 56:2185-2201
- Wei Z, Zhou N, Zou L, Shi Z, Dun B, Ren G, Yao Y (2021) Soy protein alleviates malnutrition in weaning rats by regulating gut microbiota composition and serum metabolites. Front Nutr 8:774203
- Gao K, Farzi A, Ke X, Yu Y, Chen C, Chen S, Yu T, Wang H, Li Y (2022) Oral administration of Lactococcus lactis WHH2078 alleviates depressive and anxiety symptoms in mice with induced chronic stress. Food Funct 13:957-969
- Desbonnet L, Garrett L, Clarke G, Bienenstock J, Dinan TG (2008) The probiotic bifidobacteria infantis: an assessment of potential antidepressant properties in the rat. J Psychiatr Res 43:164-174
- Xu Y, Ku BS, Yao HY, Lin YH, Ma X, Zhang YH, Li XJ (2005) Antidepressant effects of curcumin in the forced swim test and olfactory bulbectomy models of depression in rats. Pharmacol Biochem Behav 82:200-206
- Roth W, Zadeh K, Vekariya R, Ge Y, Mohamadzadeh M (2021) Tryptophan metabolism and gut-brain homeostasis. Int J Mol Sci 22:2973
- Réus GZ, Jansen K, Titus S, Carvalho AF, Gabbay V, Quevedo J (2015) Kynurenine pathway dysfunction in the pathophysiology and treatment of depression: evidences from animal and human studies. J Psychiatr Res 68:316-328
- Samad N, Yasmin F, Manzoor N (2019) Biomarkers in drug free subjects with depression: correlation with tryptophan. Psychiatry Investig 16:948-953
- Ogyu K, Kubo K, Noda Y, Iwata Y, Tsugawa S, Omura Y, Wada M, Tarumi R, Plitman E, Moriguchi S, Miyazaki T, Uchida H, Graff-Guerrero A, Mimura M, Nakajima S (2018) Kynurenine pathway in depression: a systematic review and meta-analysis. Neurosci Biobehav Rev 90:16-25
- Perkins MN, Stone TW (1982) An iontophoretic investigation of the actions of convulsant kynurenines and their interaction with the endogenous excitant quinolinic acid. Brain Res 247:184-187
- Kindler J, Lim CK, Weickert CS, Boerrigter D, Galletly C, Liu D, Jacobs KR, Balzan R, Bruggemann J, O'Donnell M, Lenroot R, Guillemin GJ, Weickert TW (2020) Dysregulation of kynurenine metabolism is related to proinflammatory cytokines, attention, and prefrontal cortex volume in schizophrenia. Mol Psychiatry 25:2860-2872
- Miller GM (2011) The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity. J Neurochem 116:164-176
- Zucchi R, Chiellini G, Scanlan TS, Grandy DK (2006) Trace amine-associated receptors and their ligands. Br J Pharmacol 149:967-978
- Grandy DK, Miller GM, Li JX (2016) "TAARgeting Addiction"--the Alamo bears witness to another revolution: an overview of the plenary symposium of the 2015 Behavior, Biology and Chemistry Conference. Drug Alcohol Depend 159:9-16
- Gainetdinov RR, Hoener MC, Berry MD (2018) Trace amines and their receptors. Pharmacol Rev 70:549-620
- Carneiro-Nascimento S, Powell W, Uebel M, Buerge M, Sigrist H, Patterson M, Pryce CR, Opacka-Juffry J (2021) Region- and receptor-specific effects of chronic social stress on the central serotonergic system in mice. IBRO Neurosci Rep 10:8-16
- Martín-Hernández D, Pereira MP, Tendilla-Beltrán H, Madrigal JLM, García-Bueno B, Leza JC, Caso JR (2019) Modulation of monoaminergic systems by antidepressants in the frontal cortex of rats after chronic mild stress exposure. Mol Neurobiol 56:7522-7533
- Le François B, Soo J, Millar AM, Daigle M, Le Guisquet AM, Leman S, Minier F, Belzung C, Albert PR (2015) Chronic mild stress and antidepressant treatment alter 5-HT1A receptor expression by modifying DNA methylation of a conserved Sp4 site. Neurobiol Dis 82:332-341
- Iyo AH, Kieran N, Chandran A, Albert PR, Wicks I, Bissette G, Austin MC (2009) Differential regulation of the serotonin 1A transcriptional modulators five prime repressor element under dual repression-1 and nuclear-deformed epidermal autoregulatory factor by chronic stress. Neuroscience 163:1119-1127
- Celada P, Puig MV, Casanovas JM, Guillazo G, Artigas F (2001) Control of dorsal raphe serotonergic neurons by the medial prefrontal cortex: involvement of serotonin-1A, GABA(A), and glutamate receptors. J Neurosci 21:9917-9929





